Thread on our new state of the science review on #LongCovid. Commissioned by @TheLancet, peer-reviewed, coauthored with @sivanmanoj, @calirunnerdoc and Janko Nikolich. Link for free access is here (after 50 days that won’t work, then you’ll have to register and use this one:
1/kwnsfk27.r.eu-west-1.awstrack.me/L0/https:%2F%2…
thelancet.com/journals/lance…
1/kwnsfk27.r.eu-west-1.awstrack.me/L0/https:%2F%2…
thelancet.com/journals/lance…
In writing this article, we wanted to get the basic science of Long COVID into dialogue with the clinical management of this condition and the patient lived experience. @calirunnerdoc brought lived experience to our author team. 2/ 

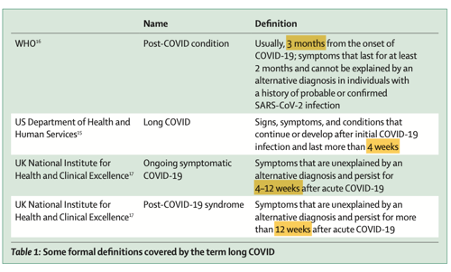
@calirunnerdoc Most but not all definitions of Long COVID put the cut-off at around 12 weeks (that is, if you’re still symptomatic 12 weeks after your initial COVID-19 infection, you’ve got Long COVID). 3/ 
A LOT of people meet this definition. In the UK, for example, almost 2% of the entire population do (grey bar to the left on this histogram). Now look at the GREEN bars. The most socio-economically deprived fifth of the population has TWICE the prevalence as the most affluent fifth. Thanks to @chrischirp for drawing this chart from @ONS data. 4/

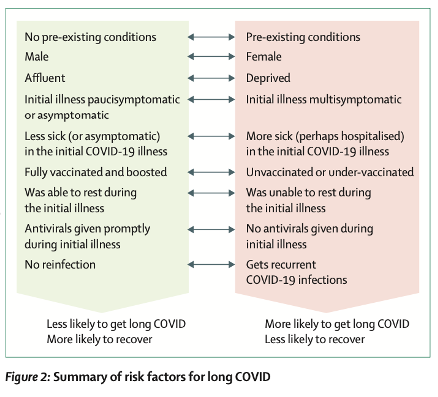
So who’s at risk? Well, all of us. But this graphic summarises the things that make you *more likely* to get Long COVID. In sum: don’t catch COVID-19. Top up your vaccines. If you do catch COVID-19, get it mildly. During acute COVID-19, rest up and if possible, take antivirals. And make sure you don’t catch it *again* since many cases of Long COVID arise from REinfections. (And also, make sure you’re male, previously healthy, and affluent). 5/
Long COVID is a multi-system disease and it sometimes seems like it causes every symptom in the book. But (and I learnt this from sitting in on Long COVID clinic heading hundreds of patient stories) there is often a *distinctive narrative* of how these symptoms fit together and fluctuate/persist/progress/resolve over time. 6/

The fatigue of Long COVID, for example, is a particular *kind* of fatigue. It’s persistent, draining, sometimes linked to triggers, and associated with sleep problems and cognitive blunting. 7/ 

Long COVID can make you unable to do your job. Go back to the histogram in tweet 4 of this thread and look at the purple bars. Six percent of people who are “inactive, not looking for work” have Long COVID. This *inability to work* represents a huge human and economic/societal burden. We need to prevent it affecting more people (and help the people already suffering). 8/

The longer you’ve had Long COVID, the lower your chances of full recovery. This is why everyone with significant symptoms of this disease should be seen *promptly* for assessment and treatment. 9/ 

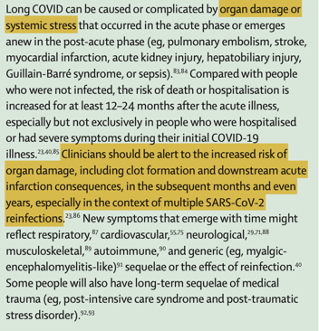
The risk of organ damage is real, and while many people do recover, serious complications can occur even months after the acute infection. (Personally, I think many heart attacks and strokes occurring in people who had COVID-19 are misclassified as ‘unrelated’ to that infection because the doctors treating them aren’t making the connection). 10/
Long COVID results from bad stuff occurring at the micro level. The literature on this is vast and confusing. Coauthor Janko Nikolitch cut through it nicely in this panel. Three PRIMARY pathological mechanisms (viral persistence, immune dysregulation, endothelial inflammation/thrombosis). 11/

These primary mechanisms then lead to all sorts of *supplementary* mechanisms including (to quote from my forthcoming Substack): release of the neurotransmitter serotonin in the brain, neurones sending signals when they shouldn’t, antibodies attacking one’s own cells, mitochondria (the energy powerhouses of cells) losing their oomph, proteins that come out wonky because they’re not folded right, deposition of some of those proteins in the muscles and other tissues, and awakening of other dormant viruses (notably Epstein-Barr, which causes glandular fever). In addition, the balance between ‘friendly’ and ‘unfriendly’ bacteria in the gut can change, with the latter getting the upper hand. 12/
Unpacking what the *primary mechanisms* are in Long COVID is crucially important for developing *mechanism-focused therapies*. We talk a lot about these in the paper. We’re not there yet with a proven therapeutic intervention but loads of ongoing studies suggest we may be on the cusp of more effective therapies. 13/

Generalist primary care clinicians (e.g. GPs) have a vital role to play in the management of this miserable condition. The opposite of gaslighting is engagement, active listening, acknowledging the story, witnessing suffering and getting your head round what’s at stake for the patient. 14/

In the paper, we have a huge table listing various symptoms along with current recommended management. Here’s the first two rows of that table. 15/ 

I had a go at summarising the whole paper in a single graphic. I’m not the world’s best artist so if someone wants to play with this and improve it, feel free! 16/ 

Do vaccines cause Long COVID? Tweeps, the overwhelmingly most important cause of Long COVID is *catching COVID-19*. Vaccines protect you against this! But to tell it like it is, in VERY RARE instances there appears to be some link between vaccination and the development of Long COVID (we’re talking *many orders of magnitude* less common than after COVID-19 infection). The HOPE is that protein-based vaccines will be less likely to produce these rare complications. 17/

Meanwhile, the mainstay of treatment is rehabilitation therapy, particularly PACING. We don’t need any more trials comparing ‘graded exercise therapy’ (GET) to symptom-guided pacing, but we DO need more research on how to optimise the latter. 18/ 

Thanks for following this thread. Loads more in the paper. The pdf should be up on @TheLancet website soon and I’ll post a link to my lay summary on Substack shortly. 19/
@TheLancet And here’s the lay summary of our #LongCovid paper on @IndependentSage Substack! open.substack.com/pub/independen…
People are asking for a link to the pdf of our Lancet paper on #LongCovid. Here it is
pdf.sciencedirectassets.com/271074/AIP/1-s…
pdf.sciencedirectassets.com/271074/AIP/1-s…
• • •
Missing some Tweet in this thread? You can try to
force a refresh







