I see some discussion of this paper going around:
It was preprinted a while ago but since that time I have had an opportunity to talk to some plasma cells researchers and it is apparent that there is a lot of important nuance being missed 🧵nature.com/articles/s4159…
It was preprinted a while ago but since that time I have had an opportunity to talk to some plasma cells researchers and it is apparent that there is a lot of important nuance being missed 🧵nature.com/articles/s4159…
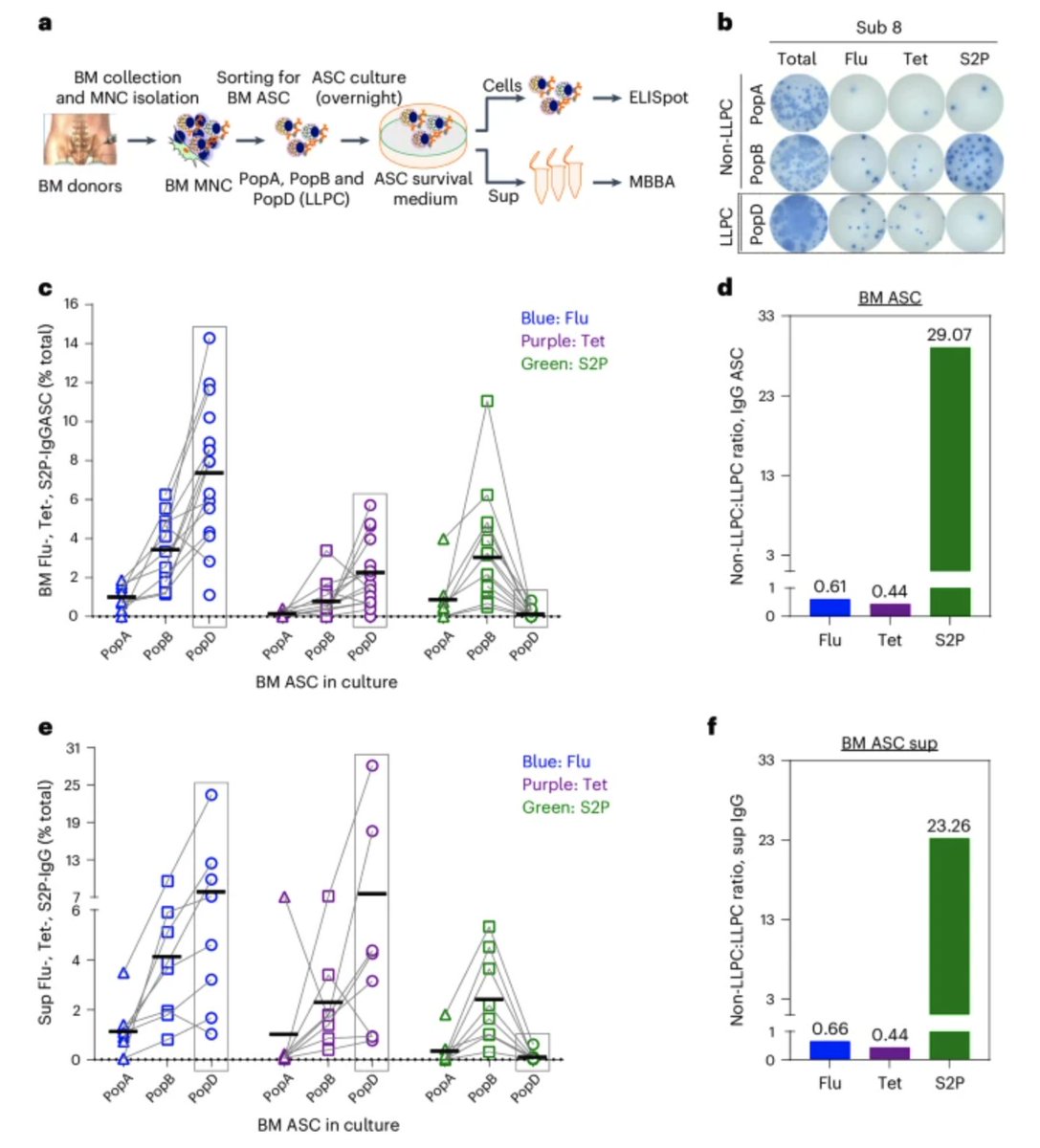
Background: antibodies against the spike protein are protective against infection by SARS-CoV-2. Antibodies are made by antibody-secreting cells (ASCs) which come from B cells and vary widely in their lifespan. The goal of vaccination is generally to elicit durable antibodies.
Long-lived plasma cells (LLPCs) are ASCs that can live for many years (potentially your lifetime). They are canonically found within the bone marrow, but mucosal LLPCs have also been described. The problem: there is no simple way to define look at a cell and say it's an LLPC.
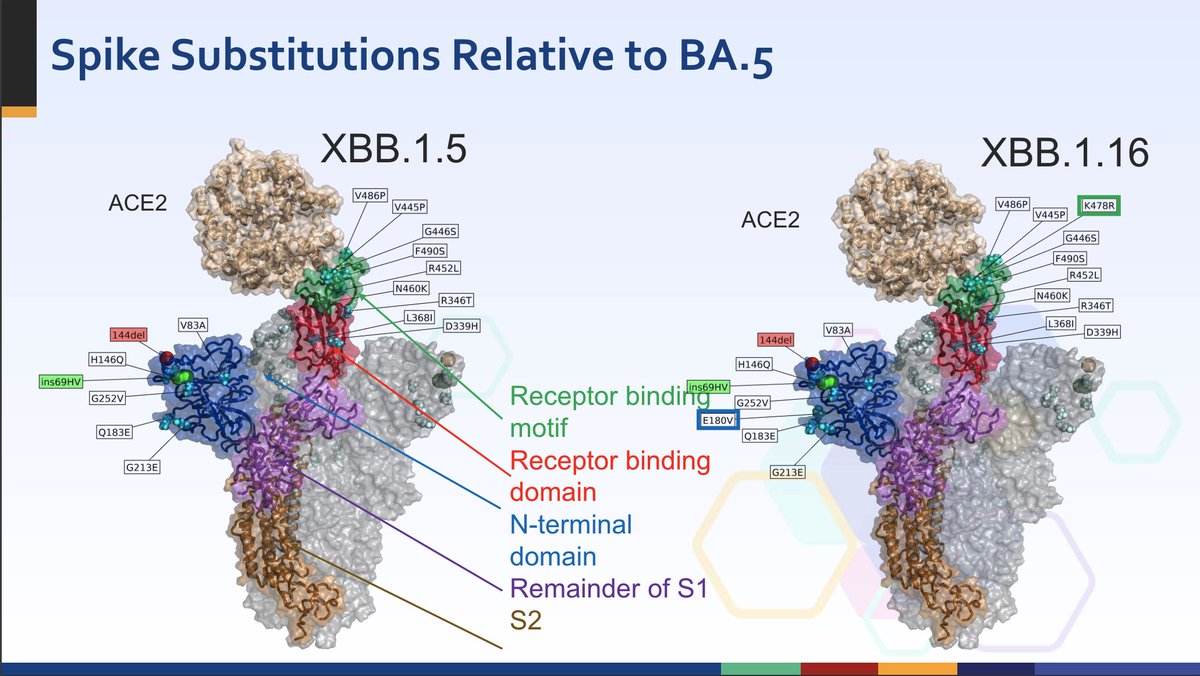
Generally different types of immune cells are defined based on what markers you find on their surface. The problem is that no set of markers uniformly defines plasma cells:
In particular, a protein called CD19 is problematic:
nature.com/articles/s4157…
sciencedirect.com/science/articl…
In particular, a protein called CD19 is problematic:
nature.com/articles/s4157…
sciencedirect.com/science/articl…
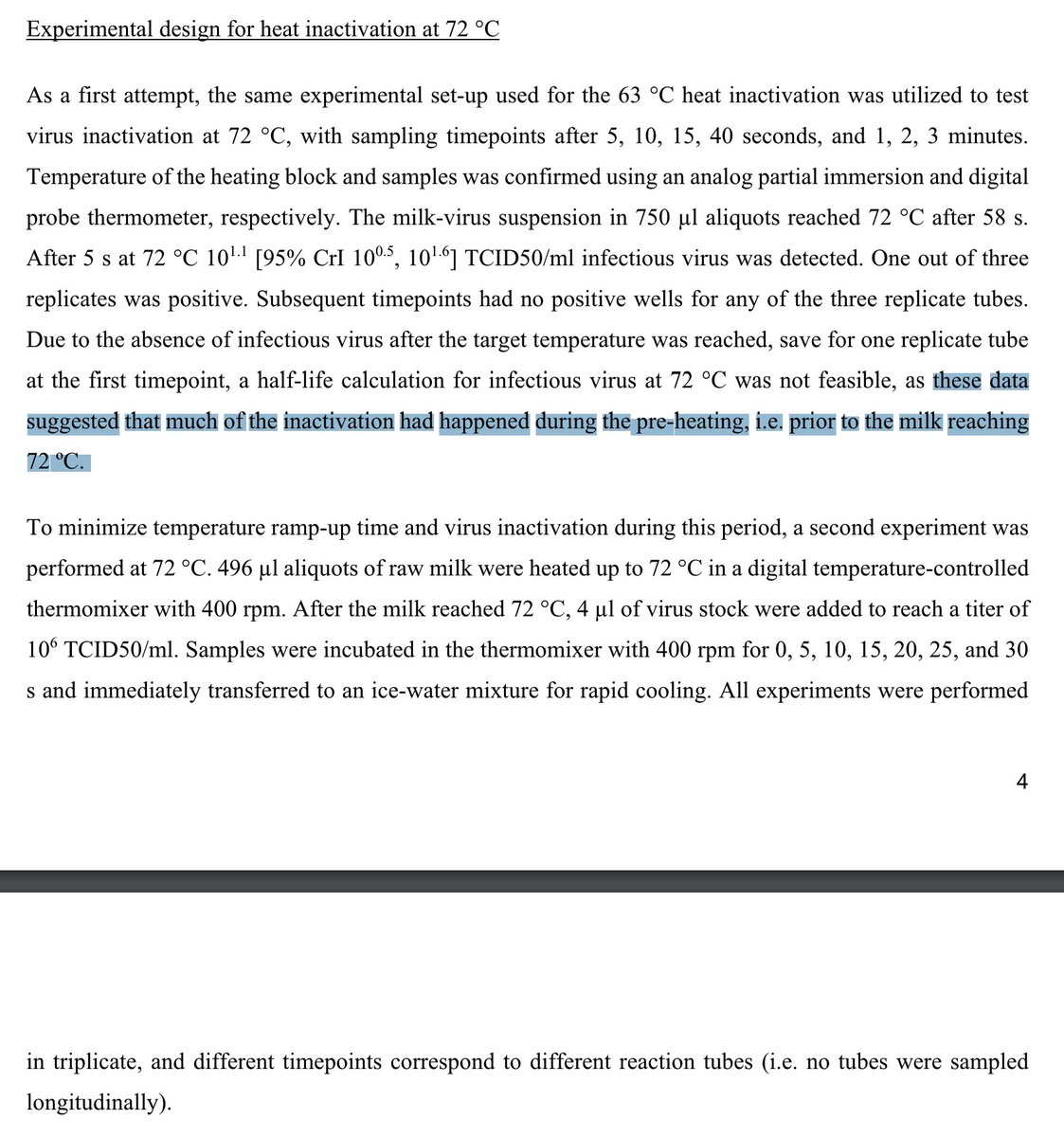
In humans, LLPCs can have CD19 or it can be absent. The team in this paper defined LLPCs as lacking CD19 (Population D). Indeed, based on this definition, there is a lack of PopD cells induced by mRNA vaccines, as well as infection and the combination.



The thing is: other literature does find that antibody levels do undergo contraction after exposure to spike by vaccination, but they are stably maintained:
Another study found bone marrow ASCs 17 months after vaccination:
sciencedirect.com/science/articl…
thelancet.com/journals/ebiom…

Another study found bone marrow ASCs 17 months after vaccination:
sciencedirect.com/science/articl…
thelancet.com/journals/ebiom…
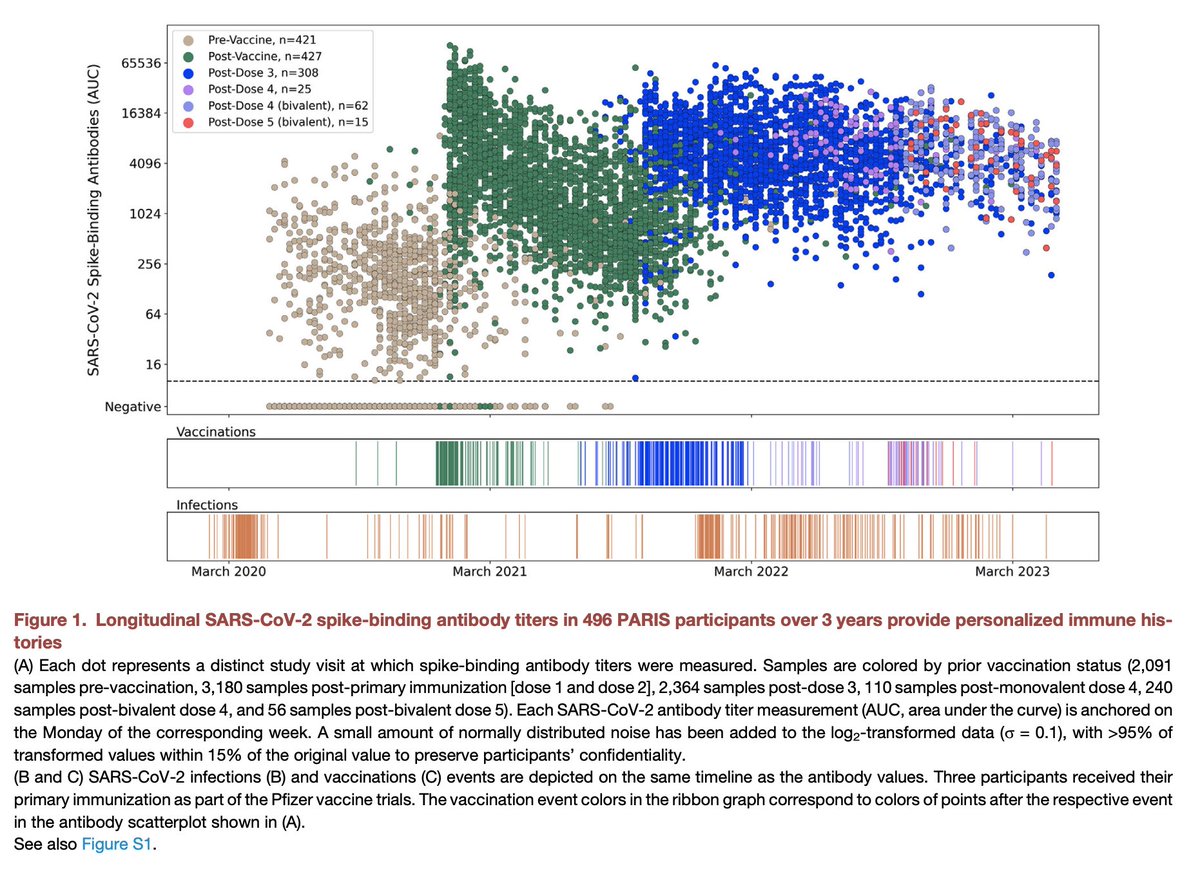
Thus even though they might not fit into the precise box of markers chosen here to define an LLPC, it is clear that there is induction of ASCs that can persist for quite a while after vaccination. But there is another question that needs to be asked- does this matter?
One of the comparators for bone marrow ASCs used by this team was influenza. You will notice they have tons of LLPCs (PopD). Yet we still get reinfected with flu all the time. It still has a substantial public health burden. We still need regular reminders for our immune system.
Like influenza, SARS-CoV-2 is a rapidly mutating respiratory virus which people will generally experience many times throughout their life. At the end of the day, we'd probably need boosters anyway.
Still, that's not to say that there is no room for improvement.
Still, that's not to say that there is no room for improvement.
Higher antibody titers for a long period of time, so long as the antibodies have breadth, would be helpful (if they occurred at the site of infection). This, however, is hard to study because of a lack of appropriate animal models. In mice, even 1 dose of mRNA vaccine gives...
essentially permanent antibody titers at a very high level. This isn't the case for humans. This could be a direct result of the immune properties of the spike protein. For instance, in lymph nodes it is preferentially taken up by medullary macrophages:
elifesciences.org/articles/86764
elifesciences.org/articles/86764
We would generally want it to be taken up by the subcapsular sinus macrophages to support robust antibody responses:
At the same time, it could be the case that mRNA vaccines are not as good at inducing LLPCs as other platforms.nature.com/articles/s4146…
journals.aai.org/jimmunol/artic…
At the same time, it could be the case that mRNA vaccines are not as good at inducing LLPCs as other platforms.nature.com/articles/s4146…
journals.aai.org/jimmunol/artic…
This is potentially suggested by the data on RSV vaccines:
Antibody responses to the mRNA RSV vaccine fade much more quickly than those against either protein vaccine. How to optimize the immune responses from mRNA vaccines merits further study for sure.cdc.gov/vaccines/acip/…
Antibody responses to the mRNA RSV vaccine fade much more quickly than those against either protein vaccine. How to optimize the immune responses from mRNA vaccines merits further study for sure.cdc.gov/vaccines/acip/…
Nevertheless, mRNA vaccines have shown excellent protection against severe COVID-19, durable memory B and T cell responses, and a highly favorable risk-benefit profile across the population. They also reduce transmission, though not completely. This study does not change that.
I would also add that the study does highlight a key knowledge gap in what it takes to get LLPCs. Tetanus is used as an example of an antigen that elicits LLPCs, yet it has none of the properties we associate with robust LLPC induction. More needs to be learned.
*defines LLPCs, sorry
@threadreaderapp please unroll
• • •
Missing some Tweet in this thread? You can try to
force a refresh