Early 40s male with chest pain and collapse, looks horrible, SBP 80, lactate 7.
Previous large PE with pulmonary hypertension on echo 2 months ago, discharged on apixaban
POCUS on arrival shows:
Previous large PE with pulmonary hypertension on echo 2 months ago, discharged on apixaban
POCUS on arrival shows:
The POCUS findings are consistent with cor pulmonale but in view of his previous echo, how do we know this is the acute cause of his shock? Should we thrombolyse?
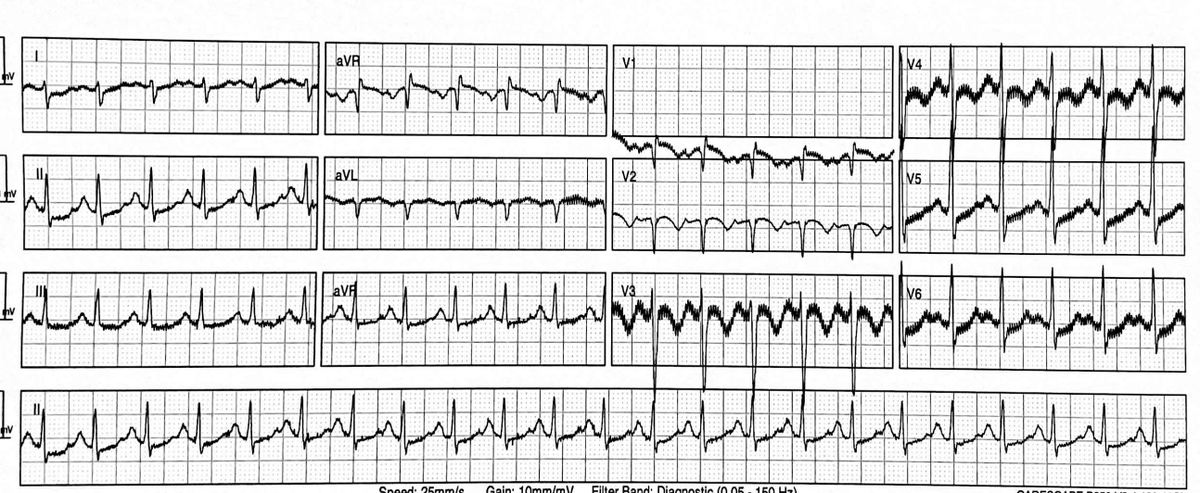
His ECG shows right axis deviation and T wave inversion. This was NEW compared with the ECGs on record from his previous admission 
Extending the POCUS down his IVC to his legs, his right common femoral vein was non-collapsible and contained echogenic material consistent with thrombus.
These data combined were enough for us to consider thrombolysis for acute massive PE
These data combined were enough for us to consider thrombolysis for acute massive PE
While alteplase was being prepared he had a CTPA (CT scanner within ED), confirming large bilateral pulmonary emboli




He was returned to Resus and consented for thrombolysis and advised of potential risk of haemorrhage including intracranial and pulmonary (because of the infarcts)
He was started on peripheral noradrenaline/norepinephrine but continued to deteriorate. He was given nebulised (iv) GTN 5mg then nebulised (iv) milrinone 5mg according to our non-official, not-publicly-endorsed evidence-sparse crashing PE quick reference guide 

A femoral arterial line was placed under US guidance
He was placed on high flow nasal cannula oxygen FiO2 1.0, 30 l/min, not because his SpO2 was low, but because oxygen is a pulmonary vasodilator
The noradrenaline was increased
He was placed on high flow nasal cannula oxygen FiO2 1.0, 30 l/min, not because his SpO2 was low, but because oxygen is a pulmonary vasodilator
The noradrenaline was increased
His BP, conscious level, and lactate improved. He was transferred to the ICU on 0.08 mcg/kg/min iv noradrenaline with a SBP of 105, MAP>65
The alteplase was still running (2 hr front loaded protocol)
The alteplase was still running (2 hr front loaded protocol)
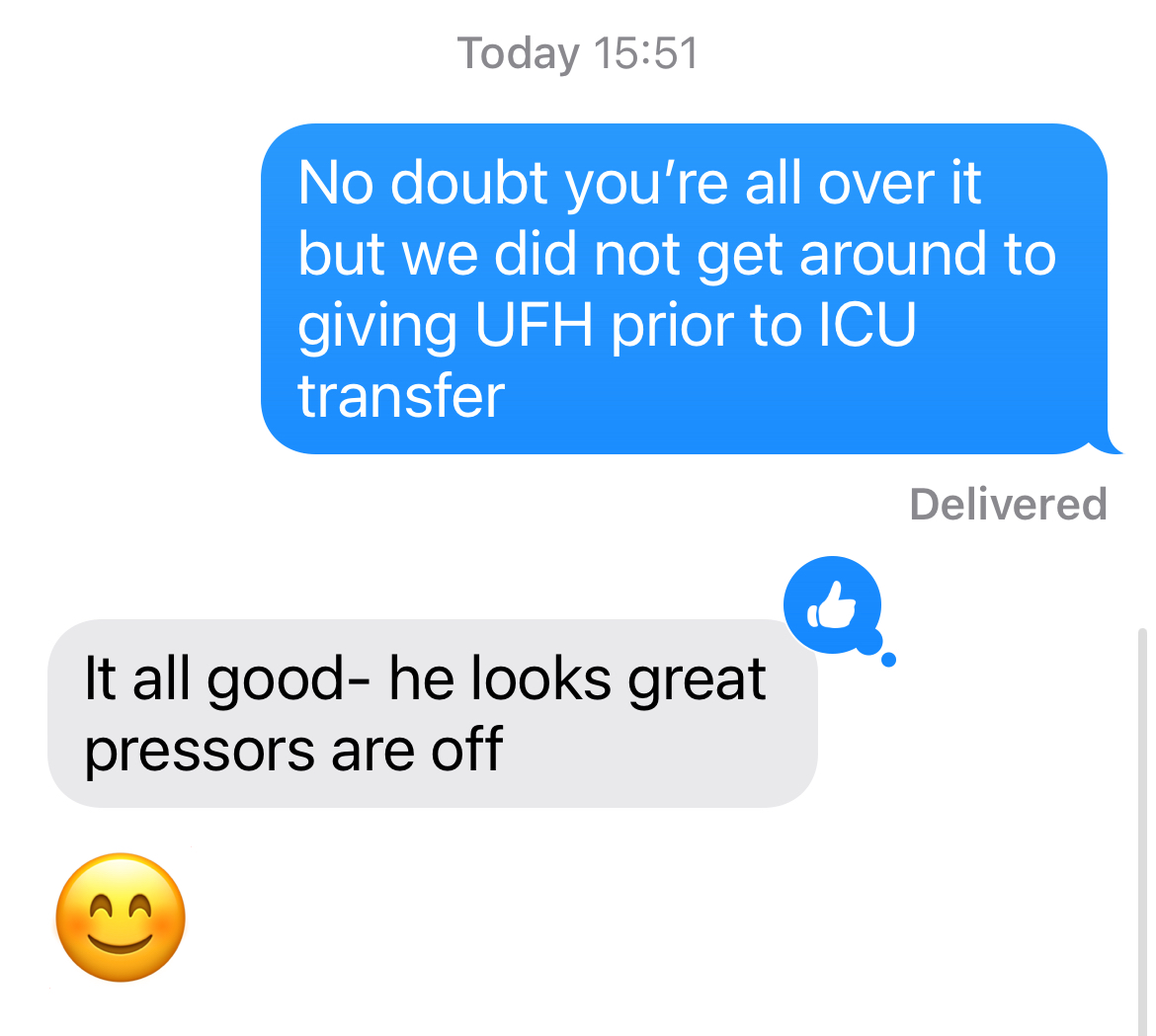
Mindful that he'd gone to ICU before we'd started unfractionated heparin, I sent a text message to the intensivist to let her know he hadn't had heparin
This was her reply
This was her reply
The team did a great job saving this patient's life. It illustrates a few important learning points:
1. Cardiac POCUS is essential in the immediate assessment of patients with undifferentiated hypotension
2. Massive PE causes RV failure not just from mechanical obstruction due to clot, but from additional pulmonary vasoconstriction in non-occluded pulmonary arteries
A resuscitation strategy for acute RV failure includes ways to reduce RV afterload including pulmonary artery vasodilators
A resuscitation strategy for acute RV failure includes ways to reduce RV afterload including pulmonary artery vasodilators
3. Our hospital does not have access to inhaled nitric oxide and is not an ECPR centre. We had to think creatively about how we can look after a crashing RV with what we have. We've used our crashing PE quick reference guide a few times now but I stress it's not validated or offically approved by any serious body
If you want to read more about the RV and inhaled GTN & milrinone, read this fantastic post by @PulmCrit emcrit.org/ibcc/pulmvaso/
Thanks for reading this resus case!
• • •
Missing some Tweet in this thread? You can try to
force a refresh


















