What if I told you…
Your body can remember.
Not just your brain.
Your kidneys, your immune cells, even your skin…
New research shows memory isn’t just something that happens in your mind.
It’s happening all throughout your body.
Let me explain (this will change how you think about stress, habits, and healing).
Your body can remember.
Not just your brain.
Your kidneys, your immune cells, even your skin…
New research shows memory isn’t just something that happens in your mind.
It’s happening all throughout your body.
Let me explain (this will change how you think about stress, habits, and healing).

For a long time, science believed memory lived only in the brain.
You experience something → neurons store it → synapses strengthen with repetition.
This is how we learn, form habits, and recall the past.
Until recently, that was the full story.
You experience something → neurons store it → synapses strengthen with repetition.
This is how we learn, form habits, and recall the past.
Until recently, that was the full story.
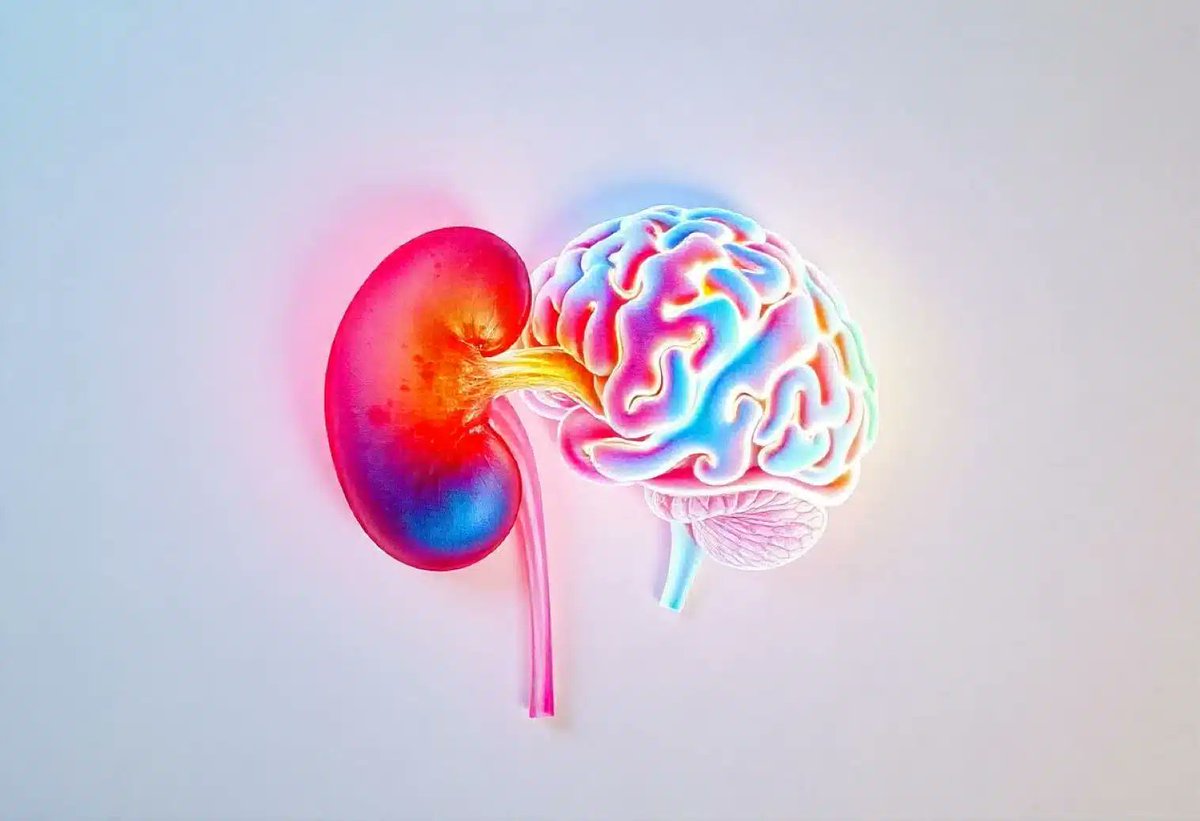
But in 2024, something surprising changed that.
A team from MIT and the Picower Institute for Learning and Memory ran a study.
They weren’t looking at brain cells.
They were studying kidney and peripheral nerve cells, the kind you’d never associate with memory.
A team from MIT and the Picower Institute for Learning and Memory ran a study.
They weren’t looking at brain cells.
They were studying kidney and peripheral nerve cells, the kind you’d never associate with memory.

What they found shocked even the researchers.
When these non-brain cells were exposed to repeated signals (like tiny patterns of input)...
They responded just like neurons do when they learn.
When these non-brain cells were exposed to repeated signals (like tiny patterns of input)...
They responded just like neurons do when they learn.
They activated a key gene called CREB, which is central to memory formation in the brain.
In short:
These cells were learning.
Here’s the really interesting part:
They used a special glowing protein, luciferase, to track this.
In short:
These cells were learning.
Here’s the really interesting part:
They used a special glowing protein, luciferase, to track this.

Luciferase lights up when memory-like activity increases.
So the more the cells "learned" the repeated pattern…
The brighter they glowed.
When memory-related pathways like ERK and CREB were blocked?
No glow.
No memory.
So the more the cells "learned" the repeated pattern…
The brighter they glowed.
When memory-related pathways like ERK and CREB were blocked?
No glow.
No memory.
This learning process followed the spacing effect, something you might know from studying.
It’s the idea that spaced-out repetition creates stronger, longer-lasting memories.
Turns out:
Kidney cells learned better when information was spaced out too.
Just like your brain.
It’s the idea that spaced-out repetition creates stronger, longer-lasting memories.
Turns out:
Kidney cells learned better when information was spaced out too.
Just like your brain.
So what does this all mean?
It doesn’t mean your kidneys are having thoughts.
But it does mean that memory-like behavior exists outside the brain.
Your body, in its own way, learns from what it experiences repeatedly.
It doesn’t mean your kidneys are having thoughts.
But it does mean that memory-like behavior exists outside the brain.
Your body, in its own way, learns from what it experiences repeatedly.
This could reshape how we understand healing, stress, disease, and even habit change.
Let’s take stress, for example.
We often think of stress as “mental.”
But chronic, repeated stress, like ongoing conflict or burnout, can affect your entire body.
Let’s take stress, for example.
We often think of stress as “mental.”
But chronic, repeated stress, like ongoing conflict or burnout, can affect your entire body.
Your cells start to "remember" those patterns.
They adapt by changing how they react to future stress.
Not just emotionally.
Biologically.
Researchers found the same memory pathways (CREB and ERK) activate in chronic stress conditions.
They adapt by changing how they react to future stress.
Not just emotionally.
Biologically.
Researchers found the same memory pathways (CREB and ERK) activate in chronic stress conditions.
When stress comes in repeated waves (as it often does), your cells begin to respond faster.
This can lead to:
– Faster cortisol spikes
– Weakened immunity
– Chronic inflammation
Not just from thoughts. From cellular conditioning.
But here’s the good news:
This can lead to:
– Faster cortisol spikes
– Weakened immunity
– Chronic inflammation
Not just from thoughts. From cellular conditioning.
But here’s the good news:
If repeated negative signals shape your body…
So do positive ones.
Think about what you do consistently:
– Practicing gratitude
– Getting restful sleep
– Moving your body
– Spending time with people you love
These aren’t just “feel-good” habits.
So do positive ones.
Think about what you do consistently:
– Practicing gratitude
– Getting restful sleep
– Moving your body
– Spending time with people you love
These aren’t just “feel-good” habits.

They help retrain your biology.
It’s not about perfection.
It’s about what you repeat.
Your body is constantly learning from what you expose it to:
– The food you eat
– The people you're around
– The routines you keep
– Even your internal dialogue
It’s not about perfection.
It’s about what you repeat.
Your body is constantly learning from what you expose it to:
– The food you eat
– The people you're around
– The routines you keep
– Even your internal dialogue
Repetition doesn’t just change your mind.
It shapes your cells.
So next time you feel stuck, burned out, or overwhelmed…
Remember this:
You are not just a brain in a body.
You are a network of learning systems.
It shapes your cells.
So next time you feel stuck, burned out, or overwhelmed…
Remember this:
You are not just a brain in a body.
You are a network of learning systems.

A living story of what you've practiced, physically and mentally.
And that means you can reshape those patterns too.
This research doesn't mean your organs are conscious.
But it does mean your body is always adapting.
And that means you can reshape those patterns too.
This research doesn't mean your organs are conscious.
But it does mean your body is always adapting.
Science is showing us that the line between mind and body is much thinner than we thought.
Your brain is learning.
Your cells are listening.
Your body is changing with every repeated input.
So be kind to it.
Choose your exposures wisely.
Your brain is learning.
Your cells are listening.
Your body is changing with every repeated input.
So be kind to it.
Choose your exposures wisely.
• • •
Missing some Tweet in this thread? You can try to
force a refresh