Medical societies have replaced merit, empiricism, and open inquiry with fashionable political orthodoxies advanced under the banner of social justice, argues a new paper in the American Journal of Medicine. Our experience with @AmerAcadPeds supports this troubling observation:🧵

Medical societies are accountable to their members, yet they often ignore their members' preferences, instead superimposing their own agendas, the authors point out.
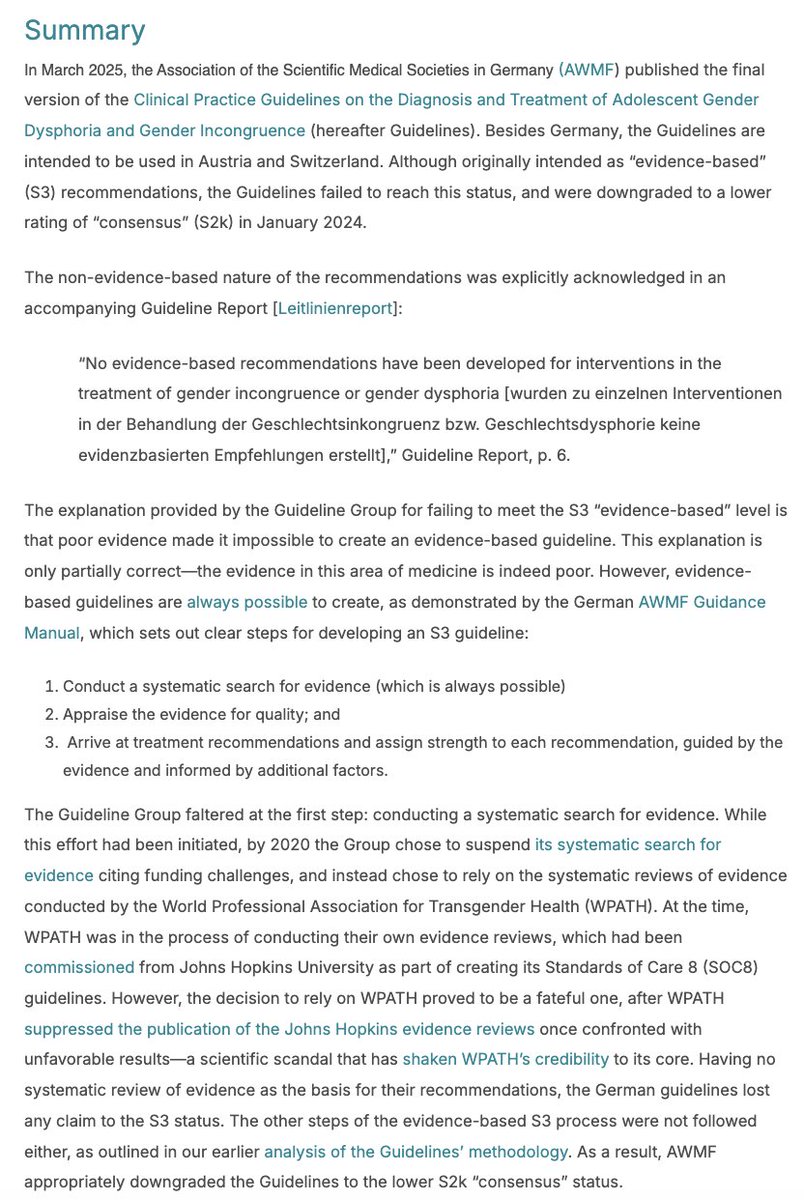
SEGM's @JuliaMasonMD1 experienced this first-hand when she, along with a group of fellow pediatricians, tried to convince the @AmerAcadPeds to align its recommendations for treating gender-dysphoric youth with systematic reviews of evidence. The AAP policy promotes gender transition of minors as the first-line treatment of gender dysphoria, yet systematic reviews do not find any trustworthy evidence of benefit of youth transitions.
While short- or long-term benefits are uncertain, biological harms such as infertility/sterility, bone health impairment, and likely adverse effects on brain development are much more certain. /2
SEGM's @JuliaMasonMD1 experienced this first-hand when she, along with a group of fellow pediatricians, tried to convince the @AmerAcadPeds to align its recommendations for treating gender-dysphoric youth with systematic reviews of evidence. The AAP policy promotes gender transition of minors as the first-line treatment of gender dysphoria, yet systematic reviews do not find any trustworthy evidence of benefit of youth transitions.
While short- or long-term benefits are uncertain, biological harms such as infertility/sterility, bone health impairment, and likely adverse effects on brain development are much more certain. /2

For several years, a group of pediatricians committed to the long-term health and well-being of gender-dysphoric youth followed AAP's due process to introduce resolutions calling on their medical society to evaluate the evidence and to update its outdated, non-evidence-based policy.
Even when a resolution was upvoted by the majority of participating pediatricians, rising to the top-5 based on positive member engagement, the AAP leadership refused to discuss the resolution during the leadership meeting. /3
buttonslives.news/p/the-american…
wsj.com/opinion/pediat…
Even when a resolution was upvoted by the majority of participating pediatricians, rising to the top-5 based on positive member engagement, the AAP leadership refused to discuss the resolution during the leadership meeting. /3
buttonslives.news/p/the-american…
wsj.com/opinion/pediat…
Instead of supporting its democratic process, the AAP issued a letter where it represented its own members asking for a review of evidence as being political. The tone was entirely dismissive, noting that "only 57" pediatricians endorsed the resolution calling for the AAP to conduct a systematic review of evidence.
The AAP never mentioned that n=57 was among the highest number of member interactions of all resolutions that year!
Inadvertently, the AAP highlighted just how few pediatricians are actually engaged with the organization. The vast majority of its members are disengaged from the AAP entirely. /4
segm.org/sites/default/…
The AAP never mentioned that n=57 was among the highest number of member interactions of all resolutions that year!
Inadvertently, the AAP highlighted just how few pediatricians are actually engaged with the organization. The vast majority of its members are disengaged from the AAP entirely. /4
segm.org/sites/default/…

The AAP has continued to amend its rules, making it more and more challenging for its members to engage in its own democratic process. This culminated with a rule that "unsponsored resolutions," i.e., those not a priori supported by the AAP leadership, were not even displayed for the members to endorse. /5

Finally, after years of @JuliaMasonMD1 and her fellow pediatricians' advocacy, the AAP promised to conduct its own systematic reviews. This was in 2023, and there is still no evidence of this happening.
To date, the AAP has simply re-affirmed its old 2018 policy that supports youth transitions uncritically. /6
publications.aap.org/aapnews/news/2…
To date, the AAP has simply re-affirmed its old 2018 policy that supports youth transitions uncritically. /6
publications.aap.org/aapnews/news/2…
The authors of the new publication explain that such excesses by medical societies have "provoked a potent reaction—from the Trump Administration, conservative state legislatures, lay advocacy groups and disaffected professionals."
Although the authors don't explicitly discuss the US medical societies' promotion of pediatric gender transitions, the article closely mirrors what has, in fact, occurred in this contentious area of medicine.
SEGM's co-founders warned of this in early 2023, writing:
"the field of gender medicine has a short time to self-correct before a growing number of authorities step in and impose guardrails to safeguard youth." /7
tandfonline.com/doi/full/10.10…
Although the authors don't explicitly discuss the US medical societies' promotion of pediatric gender transitions, the article closely mirrors what has, in fact, occurred in this contentious area of medicine.
SEGM's co-founders warned of this in early 2023, writing:
"the field of gender medicine has a short time to self-correct before a growing number of authorities step in and impose guardrails to safeguard youth." /7
tandfonline.com/doi/full/10.10…
The authors of the new publication believe that the path forward lies in the restoration of professional integrity of medical societies. "Professional organizations must reclaim their founding purpose—to advance expertise, promote inquiry, and safeguard academic freedom. Their credibility rests on competence and candor, not conformity."
SEGM agrees. We believe that the medical establishment can, and eventually will, self-correct. This is why we continue to work with major research universities, medical schools, and medical societies to promote discussion and debate. /8
SEGM agrees. We believe that the medical establishment can, and eventually will, self-correct. This is why we continue to work with major research universities, medical schools, and medical societies to promote discussion and debate. /8

SEGM's professional engagements and research & education partnerships with academic institutions, medical schools, and medical societies have come under intense pressures. Our work within the medical establishment threatens those committed to maintaining the highly politicized status quo./9
The authors of the new American Journal of Medicine's article argue that suppression of debate does not strengthen public health; it erodes confidence in it, ultimately harming patient health:
"When medicine becomes a proxy battlefield for partisan conflict, both science and patients may suffer."
The full text of the article is available at the link below. /end
amjmed.com/article/S0002-…
"When medicine becomes a proxy battlefield for partisan conflict, both science and patients may suffer."
The full text of the article is available at the link below. /end
amjmed.com/article/S0002-…
• • •
Missing some Tweet in this thread? You can try to
force a refresh