Excellent new paper by Tim Henrich et al on the bacterial, fungal, and viral infections & reactivations associated with #LongCovid.
"Various viral, bacterial, and fungal co-infections may induce or facilitate the development of PASC."
1/pmc.ncbi.nlm.nih.gov/articles/PMC12…
"Various viral, bacterial, and fungal co-infections may induce or facilitate the development of PASC."
1/pmc.ncbi.nlm.nih.gov/articles/PMC12…
44 countries have experienced a 10-fold increase in at least 13 infectious diseases compared to pre-pandemic rates, including RSV, cholera, measles, influenza, chickenpox, tuberculosis (TB), and others. 2/ 
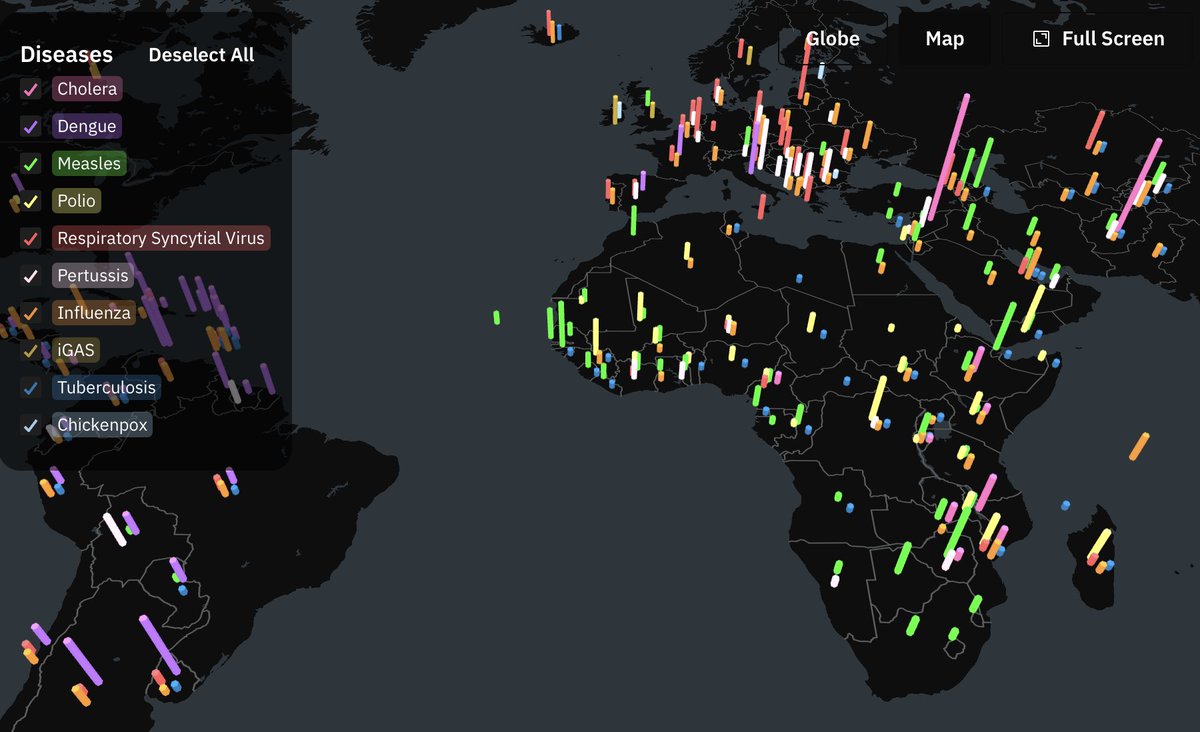
While some (like TB) may be related to declining vaccination rates, COVID impacts the others.
"Immune mechanisms [like] a period of increased vulnerability to other infections following acute COVID infection" is a major contributor, esp irt respiratory infections in children 3/
"Immune mechanisms [like] a period of increased vulnerability to other infections following acute COVID infection" is a major contributor, esp irt respiratory infections in children 3/
"Hyperinflammation of various microbial or viral origin is often followed by a period of immune suppression...#LongCovid in children has been reported to give rise to prolonged periods of innate immune hyporesponsiveness." 4/
"SARS-CoV-2-induced immune dysregulation may increase susceptibility to other infections. Conversely, increased incidence of other infections may directly induce organ dysfunction or elicit immune dysregulation, leading to persistence of SARS-CoV-2 in the tissues." 5/
Various types of co-infection can influence #LongCovid:
1) acute infections by respiratory/other pathogens (influenza, RSV, measles, adenovirus, Staphylococcus aureus, streptococci, Hemophilus spp, Moraxella spp, Klebsiella pneumoniae, Acinetobacter, Pseudomonas, Aspergillus) 6/
1) acute infections by respiratory/other pathogens (influenza, RSV, measles, adenovirus, Staphylococcus aureus, streptococci, Hemophilus spp, Moraxella spp, Klebsiella pneumoniae, Acinetobacter, Pseudomonas, Aspergillus) 6/
2) chronic infections (HIV, CMV, tuberculosis) and reactivation of latent infections (EBV, VZV, latent tuberculosis) - this includes all the herpesviruses 7/
There is a temporal component.
1) Development of #LongCovid may be affected by pre-existing and/or latent infections, via dysregulated immune responses and/or dysfunctional organ systems 9/
1) Development of #LongCovid may be affected by pre-existing and/or latent infections, via dysregulated immune responses and/or dysfunctional organ systems 9/
2) New infections and reactivation of latent infections that develop during (or soon after) acute SARS-CoV-2 infection may potentiate LC by worsening histopathology and/or immune dysregulation 10/
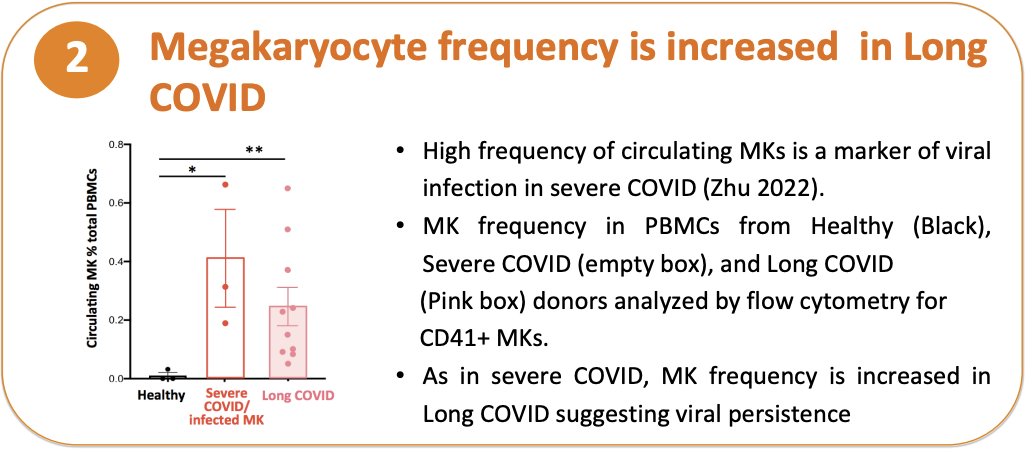
The paper goes into viral persistence, and names some of the common co-infections (viral, bacterial, and fungal) that may be involved in this process. 11/
• • •
Missing some Tweet in this thread? You can try to
force a refresh