
NAGMA Tweetorial - Got a metabolic acidosis but no anion gap? In honor of our (@curbsiders) recent RTA episode (thecurbsiders.com/internal-medic…) with @kidney_boy, here’s a quick tweetorial attempt (a la @tony_breu) on an approach to what is affectionately known as NAGMA. #5goodminutes
There are 3 commons “buckets” or categories of non anion gap metabolic acidosis: chloride intoxication, GI losses of HCO3, and renal tubular acidosis. 

The most common “bucket” of NAGMA is:
GI losses are the most common cause of NAGMA usually from profuse diarrhea though can also be from surgical drains, ureteral diversion to bowel, and medications e.g. cholestyramine.
Chloride intoxication, or, hyperchloremic metabolic acidosis, can come from heavy fluid resuscitation with normal saline. Normal saline creates a NAGMA due to chloride.
A normal serum [Cl-] is around 100 mEq/L. The chloride level is normal saline is:
The [Cl] of NS is 154 meq/L, much higher than physiological chloride levels. With heavy fluid resuscitation, chloride intoxication can cause a NAGMA. This is common in DKA patients that have no further ketones or AG but continued acidosis from the amount of fluid they received.
Can hyperchloremic acidosis cause problems? Seems so. Using “balanced” solution like ringer’s lactate instead of saline reduced major adverse kidney events by 1% in the SMART and SALTED trials NEJM 2018. See the #NephJC post for further discussion nephjc.com/news/smartsalt…
Review: NAGMA caused from 1) GI losses, 2) too much normal saline. The third is renal tubular acidosis.
What suggests some type of RTA in the setting of a metabolic acidosis?
Urine anion gap: Indirectly measures ammonium (NH4+). Remember: a “neg-GUT-ive” gap means ammonium is present and effective renal acid secretion is intact. A positive gap in the setting of metabolic acidosis suggests an RTA.
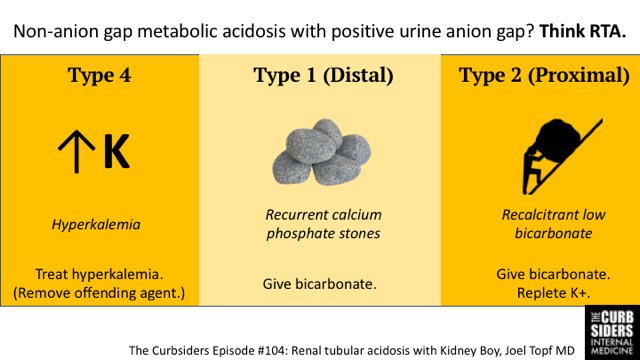
If you suspect RTA, ask: Is there hyperkalemia? If so, this is most suggestive of:
RTA 4 classically presents with mild acidosis (e.g. HCO2 22) and hyperkalemia in the setting of DM, CKD and / or medication (e.g. ACE-inhibitor). Chronic hyperkalemia of any cause leads to impaired ammoniagenesis (prevents urine buffering).
Differentiating between Proximal RTA (Type 2) and Distal RTA (Type 1) can be more difficult. Distal RTA (Type 1) is a failure to secrete H+ and is associated with:
Type 1 RTA is associated with alkalotic urine, CaPhos stones, and bone disease. Meanwhile, Proximal RTA (Type 2) is a failure to reabsorb HCO3 and creates a new “Tm" (transport maximum) for HCO3. Treatment with bicarbonate is associated with:
For RTA Type 2, patients often have persistently low bicarb and hypokalemia - they require both sodium bicarbonate and potassium salt supplementation for the hypokalemia.
A #Kashlak case: A 25yo M with recurrent calcium phosphate kidney stones presents with HCO3 of 15, no anion gap, positive urine anion gap, and hypokalemia is most consistent with:
Final #twerls: NAGMA is often 2/2 GI. Positive urine AG? RTA. RTA with hyperK? Likely Type 4. Treat the HyperK. Recurrent stones? Think RTA 1. (nb. Ca PHOSPHATE stones) Give bicarb. Hypokalemia and persistent low bicarb after bicarb tx? Think RTA 2. Give K with bicarb. 
• • •
Missing some Tweet in this thread? You can try to
force a refresh


