Thread from “Glycemic Control and Glycemic Variability in People with Type 1 Diabetes Using Open Source Artificial Pancreas Systems”, presented by Andreas Melmer, incl. @dcberne1 colleagues @ChriStettler, @thomaszueger, @markuslaimer, & @scottleibrand & @danamlewis. #ADA2019
Artificial Pancreas Systems (APS) now exist, leveraging a CGM sensor, pump, and control algorithm. Faster insulin can help, too. #ADA2019 

Traditionally, APS is developed by commercial industry, tested by clinicians, regulated, and then patients can access it. However, DIYAPS is designed by patients for individual use. #ADA2019
There are now multiple different kinds of DIYAPS systems in use: #OpenAPS, Loop, and AndroidAPS. There are differences in hardware, pump, and software configurations. The algorithm for OpenAPS is also used in AndroidAPS. #ADA2019 

DIYAPS can work offline; and also leverage the cloud for accessing or displaying data, including for remote monitoring. #ADA2019 

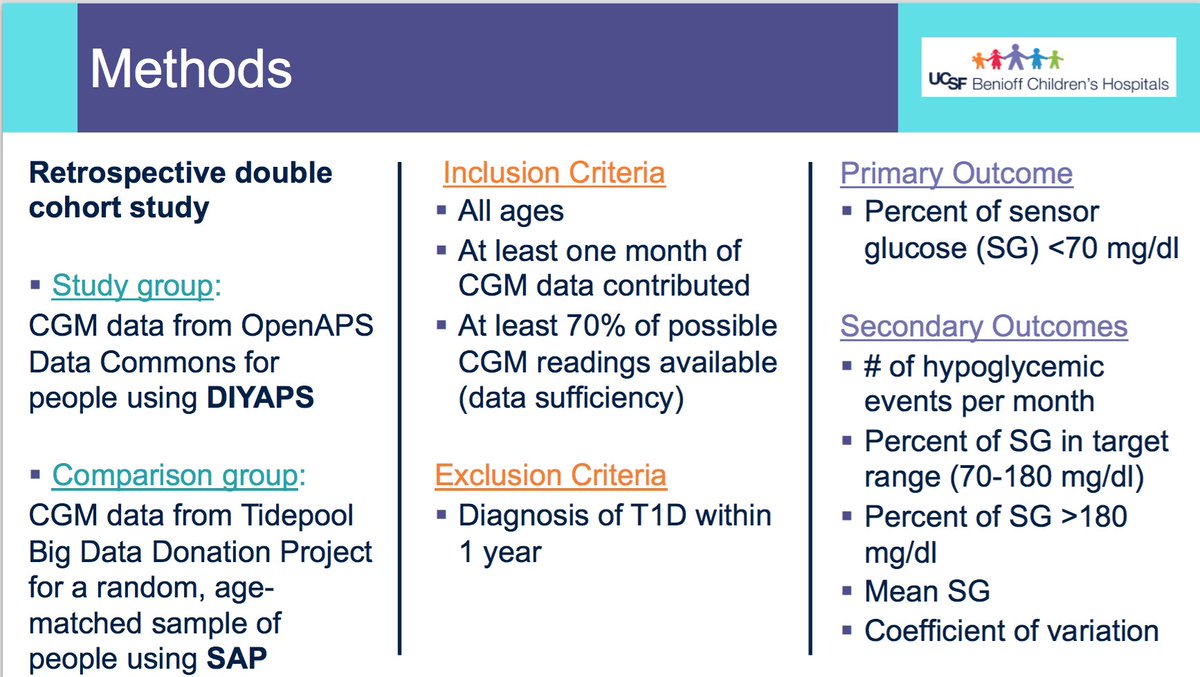
This study reviewed data from the OpenAPS Data Commons (see more here: openaps.org/data-commons/). At the time this data set was used, there were n=80 anonymized data donors from the #OpenAPS community, with a combined 53+ years worth of CGM data. #ADA2019
Looking at results for #OpenAPS data donors post-looping initiation, CV was 35.5±5.9, while eA1c was 6.4±0.7. TIR (3.9-10mmol/L) was 77.5%. Time spent >10 was 18.2%; time <3.9 was 4.3%. #ADA2019 

We selected a subcohort of n=34 who had data available from before DIY closed looping initiation (6.5 years combined of CGM records), as well as data from after (12.5 years of CGM records). #ADA2019 

For these next graphs, blue is BEFORE initiation (when just on a traditional pump); red is AFTER, when they were using DIYAPS. #ADA2019
Time in a range significantly increased for both wider (3.9-10 mmol/L) and tighter (3.9-7.8 mmol/L) ranges. #ADA2019 

Time spent out of range decreased. % time spent >10 decreased -8.3±8.6 (p<0.001); >13 decreased -3.3±5.0 (p<0.001). Change in % time spent <3.9 (-1.1±3.8 (p=0.153)), and <3.0 (-0.7±2.2 (p=0.017)) was not significant. #ADA2019 

We also analyzed daytime and nightime (the above was reflecting all 24hr combined; these graphs shows the increase in TIR and decrease in time out of range for both day and night). #ADA2019 

Also, incidence of hypoglycemic events was reduced after initiating DIYAPS. #ADA2019 

Conclusion: this was a descriptive study analyzing available CGM data from #OpenAPS Data Commons. This study shows OpenAPS has potential to support glycemic control. However, DIYAPS are currently not regulated/approved technology. Further research is recommended. #ADA2019 

(You can find a longer form copy of this presentation at bit.ly/DanaMLewisADA2…)
• • •
Missing some Tweet in this thread? You can try to
force a refresh