1/15 What are your opinions of Tweetorials?
This thread will review the results of the survey I posted from 6/28/19-7/13/19.
Thanks to everyone who completed it (n=743). If you want to see the data for yourself, the last tweet will have a link.
This thread will review the results of the survey I posted from 6/28/19-7/13/19.
Thanks to everyone who completed it (n=743). If you want to see the data for yourself, the last tweet will have a link.
2/ Demographics
Two-thirds of the respondents were doctors (41% internal medicine, 18% hospital medicine), with at least 10 other roles represented.
Nearly 80% were between 20 and 40 years old.

Two-thirds of the respondents were doctors (41% internal medicine, 18% hospital medicine), with at least 10 other roles represented.
Nearly 80% were between 20 and 40 years old.


3/ Geography
56% of respondents were from the United States, with at least one response coming from an additional 57 other countries.
The global reach of Twitter is pretty awesome.
Interactive world map: bit.ly/2xPNvhG
Interactive US map: bit.ly/2JyReHq

56% of respondents were from the United States, with at least one response coming from an additional 57 other countries.
The global reach of Twitter is pretty awesome.
Interactive world map: bit.ly/2xPNvhG
Interactive US map: bit.ly/2JyReHq


4/ What is your current level of Twitter engagement?
Unsurprisingly, many respondents were heavy consumers, with 87% using Twitter at least once/day.
Fewer people RT/like others' tweets at least once/day (67%) or post themselves (20%).
surveymonkey.com/results/SM-VLR…
Unsurprisingly, many respondents were heavy consumers, with 87% using Twitter at least once/day.
Fewer people RT/like others' tweets at least once/day (67%) or post themselves (20%).
surveymonkey.com/results/SM-VLR…

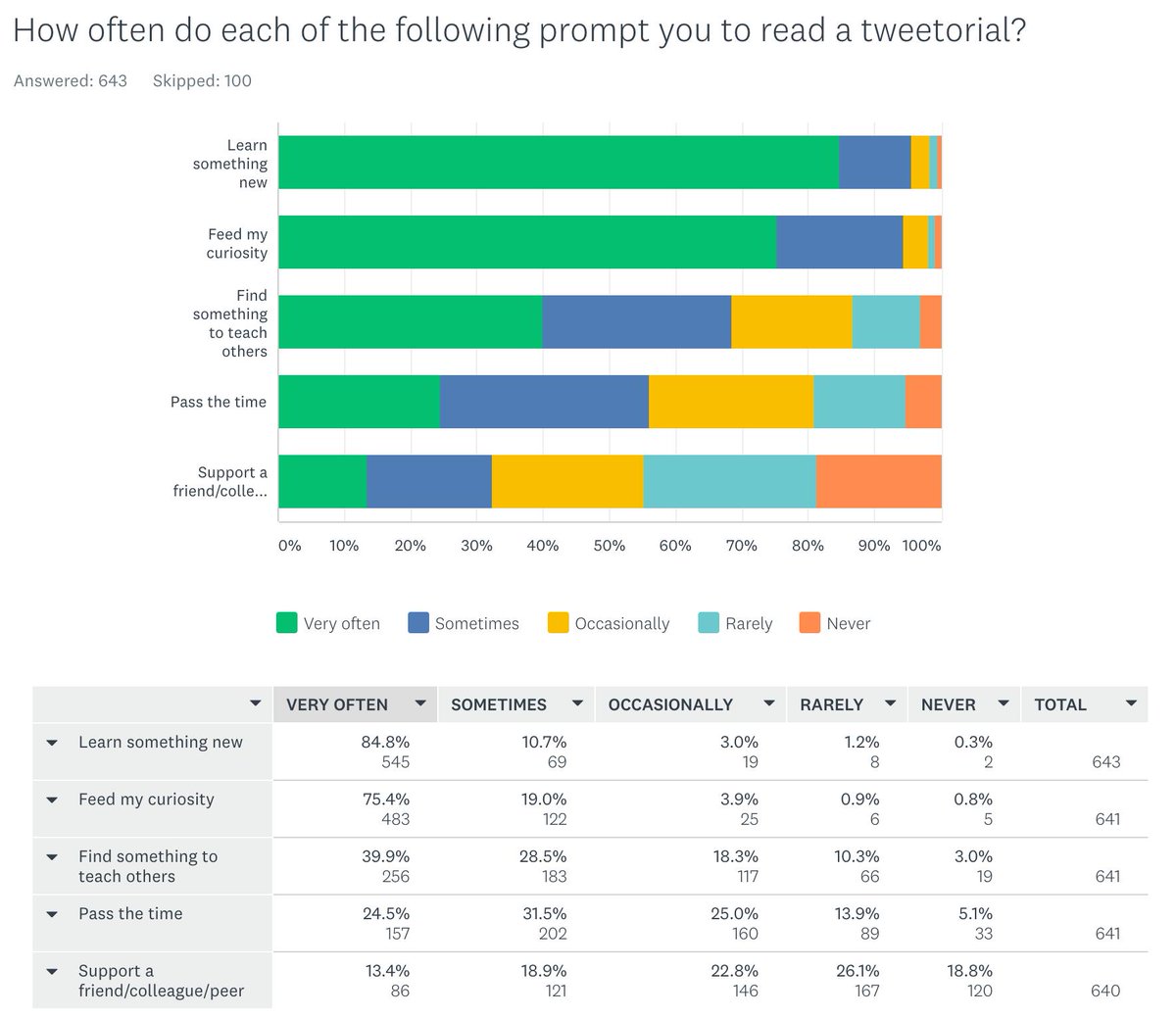
5/ How often do each of the following prompt you to read a tweetorial?
Two things "very often" drive respondents to read a tweetorial:
➣ Learn something new (85%)
➣ Feed curiosity (75%)
We are curious people!
surveymonkey.com/results/SM-6KW…
Two things "very often" drive respondents to read a tweetorial:
➣ Learn something new (85%)
➣ Feed curiosity (75%)
We are curious people!
surveymonkey.com/results/SM-6KW…
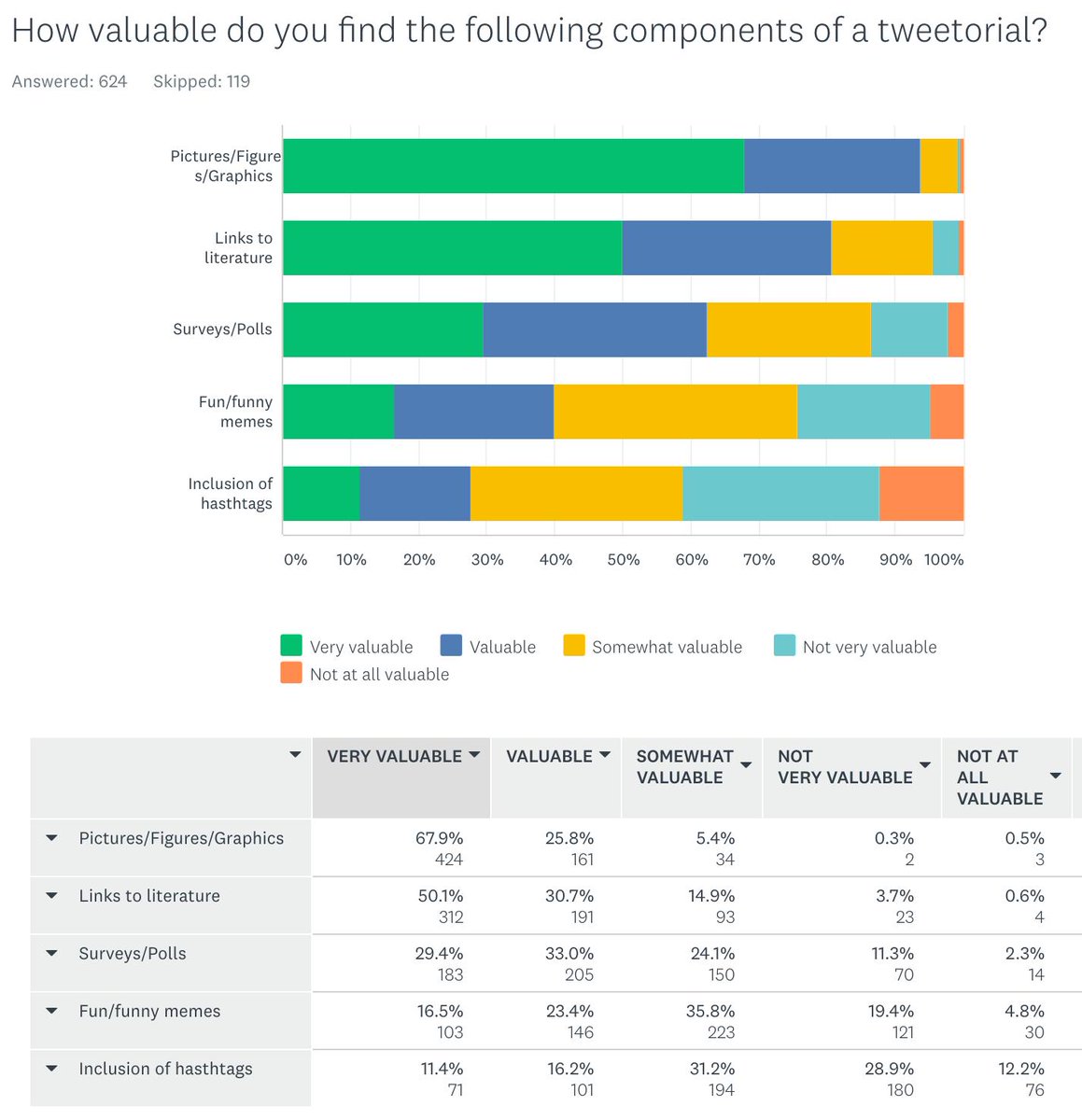
6/ How valuable do you find the following components of a tweetorial?
Three things were seen as "valuable" or "very valuable" to >50% of respondents:
➣ Pics/Figures (94%)
➣ Links to literature (81%)
➣ Surveys/Polls (63%)
One takeaway: cite your work!
surveymonkey.com/results/SM-WLF…
Three things were seen as "valuable" or "very valuable" to >50% of respondents:
➣ Pics/Figures (94%)
➣ Links to literature (81%)
➣ Surveys/Polls (63%)
One takeaway: cite your work!
surveymonkey.com/results/SM-WLF…
7/ How often do you read a tweetorial all the way through?
Most respondents (87%) "always" or "often" read a tweetorial all the way through.
What makes people stop? The number one answer (selected by 38% of respondents) was "it goes on too long”.

Most respondents (87%) "always" or "often" read a tweetorial all the way through.
What makes people stop? The number one answer (selected by 38% of respondents) was "it goes on too long”.


8/ What is the optimal tweetorial length?
Tweet 7 suggests that a tweetorial's length matters. What was the suggested optimal number of tweets?
12
Though most prefer 10-15 tweets per tweetorial, you can see from the figure that there is an audience for longer ones.
Tweet 7 suggests that a tweetorial's length matters. What was the suggested optimal number of tweets?
12
Though most prefer 10-15 tweets per tweetorial, you can see from the figure that there is an audience for longer ones.

9/
I looked at this data and didn't see any differences based on role or age.
The only thing that seemed to matter: if you "rarely" completed a tweetorial, you were more likely to prefer a shorter one, compared with those who "always" did (10 tweets versus 14).
I looked at this data and didn't see any differences based on role or age.
The only thing that seemed to matter: if you "rarely" completed a tweetorial, you were more likely to prefer a shorter one, compared with those who "always" did (10 tweets versus 14).
10/ Approximately how many times have you bookmarked or otherwise collected a tweetorial for later use?
Although 88% of respondents had read more than 5 tweetorials, few collect them. 25% had collected zero and 64% had collected 5 or fewer.
This remains an area of great need.
Although 88% of respondents had read more than 5 tweetorials, few collect them. 25% had collected zero and 64% had collected 5 or fewer.
This remains an area of great need.

11/
The free text responses support the idea that one main limitation of this platform is that content can easily be "lost".
Partially in response to this survey, I'll be working with others on the @MedTweetorials project. More information to come on this in future weeks.
The free text responses support the idea that one main limitation of this platform is that content can easily be "lost".
Partially in response to this survey, I'll be working with others on the @MedTweetorials project. More information to come on this in future weeks.
12/ Should tweetorials be peer reviewed?
33% responded yes. I did not ask a follow-up question about what this process might look like.
Also, there were no clear differences based on role or whether one has written a tweetorial.
33% responded yes. I did not ask a follow-up question about what this process might look like.
Also, there were no clear differences based on role or whether one has written a tweetorial.

13/ What is the best comparison for a tweetorial?
Nearly half (47%) see tweetorials as lectures.
Unsurprisingly, if you view a tweetorial as a form of peer-reviewed research, you're more likely to think it should be peer-reviewed (66% versus 32% for "lecture”).
Nearly half (47%) see tweetorials as lectures.
Unsurprisingly, if you view a tweetorial as a form of peer-reviewed research, you're more likely to think it should be peer-reviewed (66% versus 32% for "lecture”).

14/ Have you (how many) tweetorials have you posted?
About 1 in 7 (14%) of respondents have posted a tweetorial. That’s 82 people.
59% have written 3 or fewer with 18 having written 1.
One need not make this a full-time job to be a valuable contributor!
About 1 in 7 (14%) of respondents have posted a tweetorial. That’s 82 people.
59% have written 3 or fewer with 18 having written 1.
One need not make this a full-time job to be a valuable contributor!

15/15
Those are some of the key results of the survey.
If you're interested in reviewing the full set of anonymous data, you can see it here (I have left out free-text answers):
surveymonkey.com/results/SM-WBD…
Those are some of the key results of the survey.
If you're interested in reviewing the full set of anonymous data, you can see it here (I have left out free-text answers):
surveymonkey.com/results/SM-WBD…
Please feel free to use the results of this presentation.
If you would like to reference this tweetorial, here is a suggested citation:
Breu, AC. (@tony_breu). “What are your opinions of Tweetorials?” Twitter. 14 July 2019, 10:37 AM.
If you would like to reference this tweetorial, here is a suggested citation:
Breu, AC. (@tony_breu). “What are your opinions of Tweetorials?” Twitter. 14 July 2019, 10:37 AM.
https://twitter.com/tony_breu/status/1150414038855233536.
• • •
Missing some Tweet in this thread? You can try to
force a refresh