Last week we had our traditional lecture on Dizziness by our amazing PD, Dr @AndrewGutwein!...
As you are probably very aware, this is a very common complain!, and can have many subtleties.
1/n
#JacobiIM #JacobiNoonConference #medtwitter #FOAMed #DDx @CPSolvers @DxRxEdu
As you are probably very aware, this is a very common complain!, and can have many subtleties.
1/n
#JacobiIM #JacobiNoonConference #medtwitter #FOAMed #DDx @CPSolvers @DxRxEdu
Dizziness is VERY relative...
Patient can describe it as spinning, lightheaded, "blacking out", but sometimes, it is just "Dizziness".
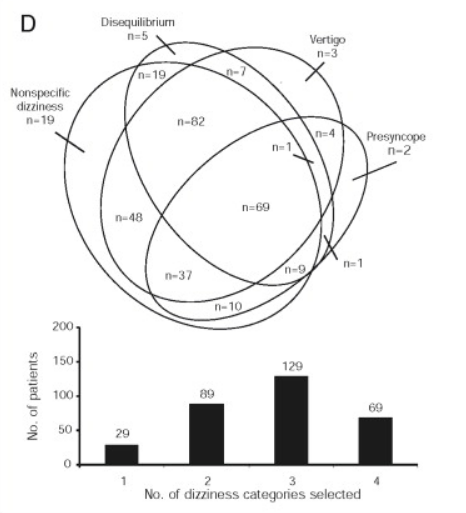
Newman et al evaluated the overlap of dizziness categories based on symptoms. (May Clin Proceedings, 2007-11-01,Vol 82,1)
2/n
#JacobiIM
Patient can describe it as spinning, lightheaded, "blacking out", but sometimes, it is just "Dizziness".
Newman et al evaluated the overlap of dizziness categories based on symptoms. (May Clin Proceedings, 2007-11-01,Vol 82,1)
2/n
#JacobiIM
But if it is just dizzy...DON'T STOP AT "JUST DIZZY"...try to really understand what is it!....As Dr Gutwein, says, "Dizziness is Meaningless".
A good way to try to understand what the patient means is:
3/n
#JacobiIM
A good way to try to understand what the patient means is:
3/n
#JacobiIM

Let's talk about a useful classification based on the etiology suggested by Dr Gutwein. Let's start with Vertigo:
4/n
#JacobiIM
4/n
#JacobiIM

Vertigo is described a sensation of 𝗺𝗼𝘁𝗶𝗼𝗻. It is usually described as a spinning sensation (either the room or the pt) but could be lateral like on a boat.
5/n
#JacobiIM
5/n
#JacobiIM
An important step is differentiating central vs peripheral vertigo. The HINTS exam is a series of bedside test that has = or > Sens as MRI for central etiology.
If none of the components of the HINTS suggest central etiology, likely it is peripheral.
6/n
#JacobiIM
If none of the components of the HINTS suggest central etiology, likely it is peripheral.
6/n
#JacobiIM

Peripheral vertigo: time course and symptoms characteristics are very helpful. The most common etiologies are BPPV and vestibular neuritis, with many other less common etiologies including Meniere's and Alternobaric vertigo (from atm pressure changes)
7/n
#JacobiIM
7/n
#JacobiIM

If you suspect BPPV, the Dix Hallpike maneuvre is a good diagnostic test. Here is a nice video from @bmj_latest showing how to perform it. Remember, it is positive if you elicit nistagmus, so it doesn't make any sense doing it if the patient already has it!
8/n
#JacobIM
8/n
#JacobIM
(Pre-) Syncope is a very broad topic, and could be a tweetorial on its own, but all the categories share:
-Not enough Blood to CNS
-Low O2 to CNS
-Low Glucose to CNS
This explain in this amazing graph by @escardio - syncope guidelines doi.org/10.1093/eurhea…
9/n
#JacobiIM
-Not enough Blood to CNS
-Low O2 to CNS
-Low Glucose to CNS
This explain in this amazing graph by @escardio - syncope guidelines doi.org/10.1093/eurhea…
9/n
#JacobiIM

@CPSolvers have an amazing approach to syncope, dividing it in 3 big categories. Again, the description of the episode is crucial, as this can point towards a specific etiology.
Features such as excertional/supine episodes, no prodrome, etc can suggest high risk
#JacobiIM
10/n
Features such as excertional/supine episodes, no prodrome, etc can suggest high risk
#JacobiIM
10/n

A good HPI/PE (including orthostatic BP), maybe a CBC and an EKG and carefull medication reconciliation can lead to a diagnosis without further work up.
Remember, cardiac etiology is the one we are concerned, it has a higher mortality.
#JacobiIM
11/n
Remember, cardiac etiology is the one we are concerned, it has a higher mortality.
#JacobiIM
11/n
Next, 𝗗𝘆𝘀𝗲𝗾𝘂𝗶𝗹𝗹𝗶𝗯𝗿𝗶𝘂𝗺.
This is usually described as 𝙞𝙢𝙗𝙖𝙡𝙖𝙣𝙘𝙚 or 𝙪𝙣𝙨𝙩𝙚𝙖𝙙𝙞𝙣𝙚𝙨𝙨. Behind it there is usually an imbalance in our sensory input. This includes our vision, propioception and sensitive input.
#JacobiIM
12/n
This is usually described as 𝙞𝙢𝙗𝙖𝙡𝙖𝙣𝙘𝙚 or 𝙪𝙣𝙨𝙩𝙚𝙖𝙙𝙞𝙣𝙚𝙨𝙨. Behind it there is usually an imbalance in our sensory input. This includes our vision, propioception and sensitive input.
#JacobiIM
12/n

This could be divided on 𝘼𝙪𝙩𝙤𝙣𝙤𝙢𝙞𝙘 𝘿𝙮𝙨𝙛𝙪𝙣𝙘𝙩𝙞𝙤𝙣, 𝘿𝙚𝙘𝙧𝙚𝙖𝙨𝙚𝙙 𝙨𝙚𝙣𝙨𝙞𝙩𝙞𝙫𝙚 𝙞𝙣𝙥𝙪𝙩 and 𝙄𝙢𝙥𝙖𝙞𝙧𝙚𝙙 𝘾𝙤𝙤𝙧𝙙𝙞𝙣𝙖𝙩𝙞𝙤𝙣/𝙎𝙩𝙧𝙚𝙣𝙜𝙝𝙩.
There is usually >1 cause, and many etiologies have >1 pathophysiology.
#JacobiIM
13/n
There is usually >1 cause, and many etiologies have >1 pathophysiology.
#JacobiIM
13/n

Again, a good history, physical exam and medication reconciliation are very important.
Although many are not amanable of being corrected (already stablish DM neuropathy), increasing the sensitive output through devices or PT can help.
#JacobiIM
14/n
Although many are not amanable of being corrected (already stablish DM neuropathy), increasing the sensitive output through devices or PT can help.
#JacobiIM
14/n
Meds can leading to dizziness in several ways. Many can decrease propioception and sensinput (as EtOH, sedatives), but lead to neuropathy/vestibular dysfunction.
Vinca alkaloids, taxanes and Oxaliplatin are some chemotherapeutic agents that can cause neuropathy
15/n
#JacobiIM
Vinca alkaloids, taxanes and Oxaliplatin are some chemotherapeutic agents that can cause neuropathy
15/n
#JacobiIM
Lastly, the "Others" category. This include less common etiologies such as CO poisoning, post-traumatic dizziness and psychogenic etiology. As this category is heterogeneous, careful exclusion of other causes should take place before any case is attributed.
16/n
#JacobiIM
16/n
#JacobiIM

Fin!. This is by no means a comprenhensive list of all causes, but rather a schema to approach to dizziness.
@CPSolvers
#JacobiIM #Tweetorial #FOAMed
@CPSolvers
#JacobiIM #Tweetorial #FOAMed
• • •
Missing some Tweet in this thread? You can try to
force a refresh






