Part 1 of 2 | MCQ in 2nd Part 2:
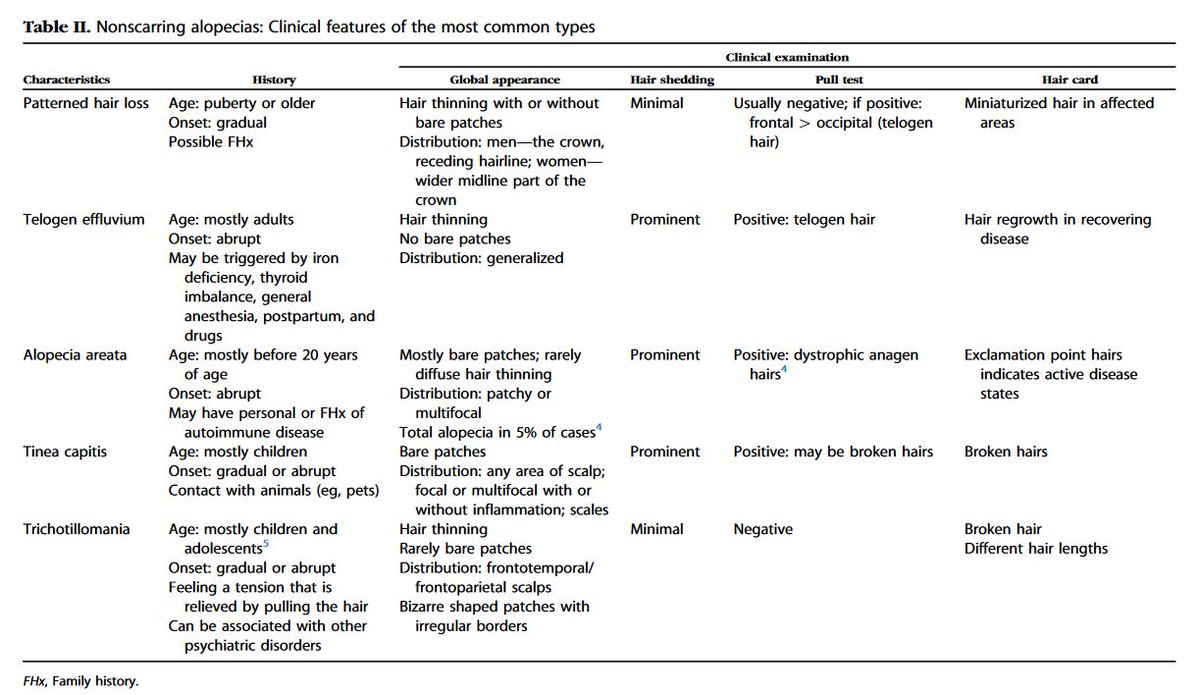
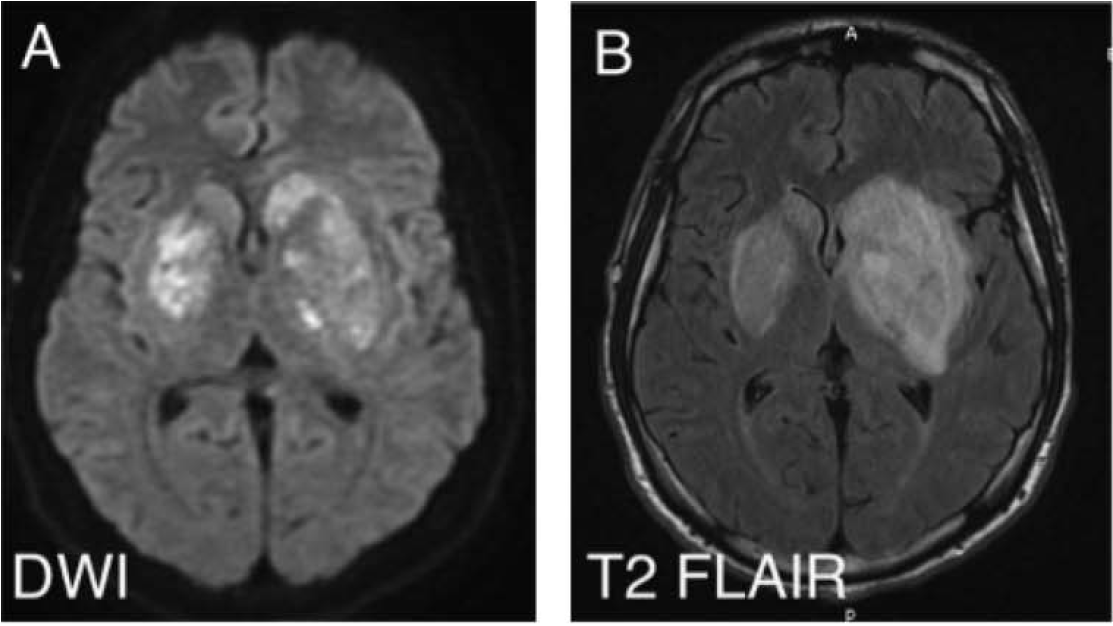
23M active IV heroin user p/w 4 d fever/headache/seizure. Temp 39.3, supple neck. Initial head CT (-). CSF: WBC 30 (60% L), TP 90, gluc n/l. Developed R arm/leg hemiparesis hospital day 5. MRI: large L>R b/l basal ganglia enhancing lesions (👇)
23M active IV heroin user p/w 4 d fever/headache/seizure. Temp 39.3, supple neck. Initial head CT (-). CSF: WBC 30 (60% L), TP 90, gluc n/l. Developed R arm/leg hemiparesis hospital day 5. MRI: large L>R b/l basal ganglia enhancing lesions (👇)
|Part 2 of 2 |
Routine CSF viral PCRs/bacterial/AFB/fungal Cxs (-). Blood Cxs, HIV, RPR, TEE (-). Lives in Missouri, no travel/other exposures. Continued to be highly febrile on cefepime/vancomycin/metronidazole. What is the most likely cause of his clinical presentation?
Routine CSF viral PCRs/bacterial/AFB/fungal Cxs (-). Blood Cxs, HIV, RPR, TEE (-). Lives in Missouri, no travel/other exposures. Continued to be highly febrile on cefepime/vancomycin/metronidazole. What is the most likely cause of his clinical presentation?
1/9
Only 37% got the correct answer, Mucor.
Learning points:
✔️ High risk of cerebral mucormycosis among people who inject drugs (PWID)
✔️ Unique basal ganglia involvement seen in these cases
Picture in MCQ taken from:
ncbi.nlm.nih.gov/pmc/articles/P…
Only 37% got the correct answer, Mucor.
Learning points:
✔️ High risk of cerebral mucormycosis among people who inject drugs (PWID)
✔️ Unique basal ganglia involvement seen in these cases
Picture in MCQ taken from:
ncbi.nlm.nih.gov/pmc/articles/P…
2/9
We've recently discussed some of the infections seen among PWID 👇
Isolated cerebral mucromycosis is one these infections clinicians need to be aware of. \
This MCQ was inspired by a case presented in our #idgrandrounds in 2015.
We've recently discussed some of the infections seen among PWID 👇
https://twitter.com/WuidQ/status/1191477822579204104?s=20
Isolated cerebral mucromycosis is one these infections clinicians need to be aware of. \
This MCQ was inspired by a case presented in our #idgrandrounds in 2015.
3/9
Common Mucor risk factors:
▪️ DM in DKA, steroids, hematologic malignancies, transplantation, neutropenia, trauma/burns
Common forms:
▪️ Rhino-orbito-cerebral | pulmonary | disseminated > GI
▪️ Cutaneous (trauma/burn)
Isolated Mucor:
▪️ Renal & cerebral seen in PWID
Common Mucor risk factors:
▪️ DM in DKA, steroids, hematologic malignancies, transplantation, neutropenia, trauma/burns
Common forms:
▪️ Rhino-orbito-cerebral | pulmonary | disseminated > GI
▪️ Cutaneous (trauma/burn)
Isolated Mucor:
▪️ Renal & cerebral seen in PWID
4/9
Isolated cerebral Mucor in PWID:
1⃣ Predilection for the basal ganglia (uni-/bi lateral)
Case series: 20 of 22 patients have basal ganglia involvement
ncbi.nlm.nih.gov/pubmed/7888545
68 patients w/ isolated cerebral Mucro 👉 82% PWID, 71% ➕basal ganglia
ncbi.nlm.nih.gov/pubmed/30415043
Isolated cerebral Mucor in PWID:
1⃣ Predilection for the basal ganglia (uni-/bi lateral)
Case series: 20 of 22 patients have basal ganglia involvement
ncbi.nlm.nih.gov/pubmed/7888545
68 patients w/ isolated cerebral Mucro 👉 82% PWID, 71% ➕basal ganglia
ncbi.nlm.nih.gov/pubmed/30415043
5/9
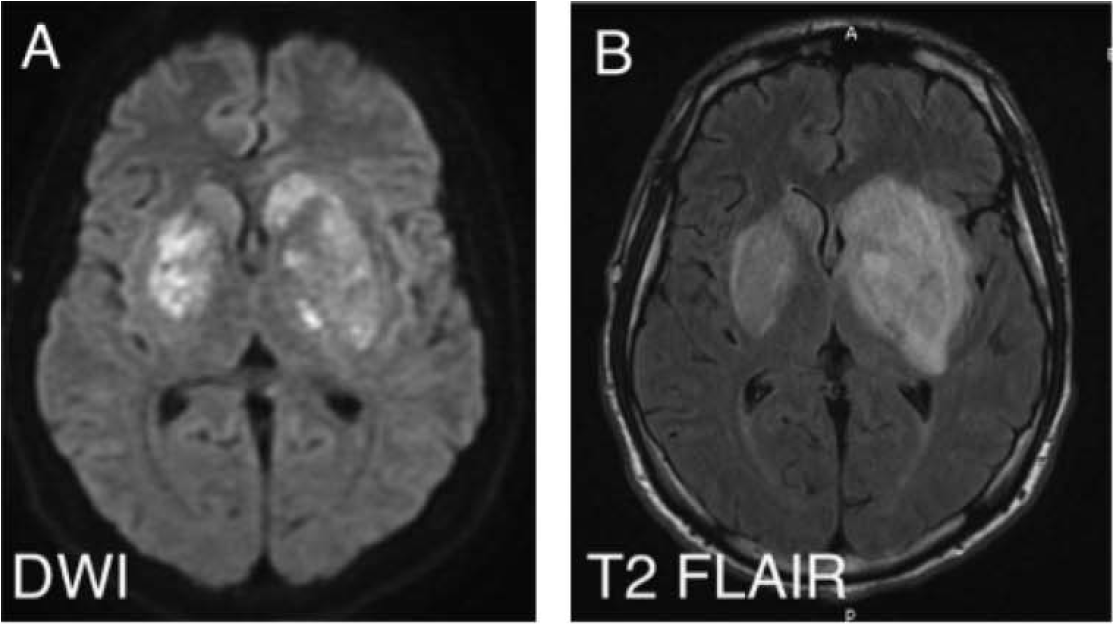
Why the basal ganglia?
Mucor, highly angioinvasive. Tissue infarction/necrosis, path hallmarks.
academic.oup.com/cid/article/45…
Contaminated injection ➕ microvascular injury from injected drug 👉 seeding to highly vascularized area (small penetrating arterioles/collaterals)
Why the basal ganglia?
Mucor, highly angioinvasive. Tissue infarction/necrosis, path hallmarks.
academic.oup.com/cid/article/45…
Contaminated injection ➕ microvascular injury from injected drug 👉 seeding to highly vascularized area (small penetrating arterioles/collaterals)
6/9
2⃣ Need to have a high index of suspicion (can lead to early dx & tx)
▪️ Can present like typical meningitis (fever, mental status change, headache); but almost 50%,➕hemiparesis
▪️ Rapidly progressive course despite abx
▪️ Brain biopsy is diagnostic (only 38% had ➕culture)
2⃣ Need to have a high index of suspicion (can lead to early dx & tx)
▪️ Can present like typical meningitis (fever, mental status change, headache); but almost 50%,➕hemiparesis
▪️ Rapidly progressive course despite abx
▪️ Brain biopsy is diagnostic (only 38% had ➕culture)
7/9
3⃣ High mortality rate
▪️ 65% mortality rate, survival a/w receipt of amphotericin & stereotactic aspiration ncbi.nlm.nih.gov/pubmed/30415043
Among 70 patients: delay in antifungals (>6 days after dx) led to a 2-fold mortality increase academic.oup.com/cid/article/47…
3⃣ High mortality rate
▪️ 65% mortality rate, survival a/w receipt of amphotericin & stereotactic aspiration ncbi.nlm.nih.gov/pubmed/30415043
Among 70 patients: delay in antifungals (>6 days after dx) led to a 2-fold mortality increase academic.oup.com/cid/article/47…
8/9
Other answers:
✔️ CNS Toxo is highly unusual in people w/o HIV/immunosuppression
✔️ Although VZV PCR can miss intracranial VZV vasculopathy, most lesions are in gray-white matter junction
✔️ Case lacks findings c/w rabies: hydrophobia, aerophobia, exposure, etc
Other answers:
✔️ CNS Toxo is highly unusual in people w/o HIV/immunosuppression
✔️ Although VZV PCR can miss intracranial VZV vasculopathy, most lesions are in gray-white matter junction
✔️ Case lacks findings c/w rabies: hydrophobia, aerophobia, exposure, etc
9/9
In summary:
▪️ Need to be aware of isolated cerebral Mucor among PWID (high index of suspicion, rapid course, stroke-like presentation, basal ganglia lesions)
▪️ Early suspicion, early Tx and Dx 👉 life saving!
In summary:
▪️ Need to be aware of isolated cerebral Mucor among PWID (high index of suspicion, rapid course, stroke-like presentation, basal ganglia lesions)
▪️ Early suspicion, early Tx and Dx 👉 life saving!
9/9 EXTRA
In patients w/ cerebral Mucor (like in this featured case), would you use high dose ampho (10 mg/kg/day)?
academic.oup.com/jac/article/70…
@FungalDoc @GermHunterMD @ShohamTxID @CarlosdelRio7 @PaulSaxMD @RazonableMD @DocWoc71 @BradCutrellMD @Cortes_Penfield
In patients w/ cerebral Mucor (like in this featured case), would you use high dose ampho (10 mg/kg/day)?
academic.oup.com/jac/article/70…
@FungalDoc @GermHunterMD @ShohamTxID @CarlosdelRio7 @PaulSaxMD @RazonableMD @DocWoc71 @BradCutrellMD @Cortes_Penfield
@FungalDoc @GermHunterMD @ShohamTxID @CarlosdelRio7 @PaulSaxMD @RazonableMD @DocWoc71 @BradCutrellMD @Cortes_Penfield Thank you for your response @FungalDoc @BradSpellberg @TxID_Edu @jdcooperid @FarhanFazal10.
I remember, this patient unfortunately expired despite higher dose ampho. By the time brain biopsy done & showed molds, might have been too late already.
I remember, this patient unfortunately expired despite higher dose ampho. By the time brain biopsy done & showed molds, might have been too late already.
• • •
Missing some Tweet in this thread? You can try to
force a refresh