
How to get URL link on X (Twitter) App



https://twitter.com/WuidQ/status/1305649807395033088?s=202/20


https://twitter.com/WuidQ/status/10192553977760235522/12
https://twitter.com/WuidQ/status/1128297551726297088


 Part 2/2 📌 [case continued]
Part 2/2 📌 [case continued]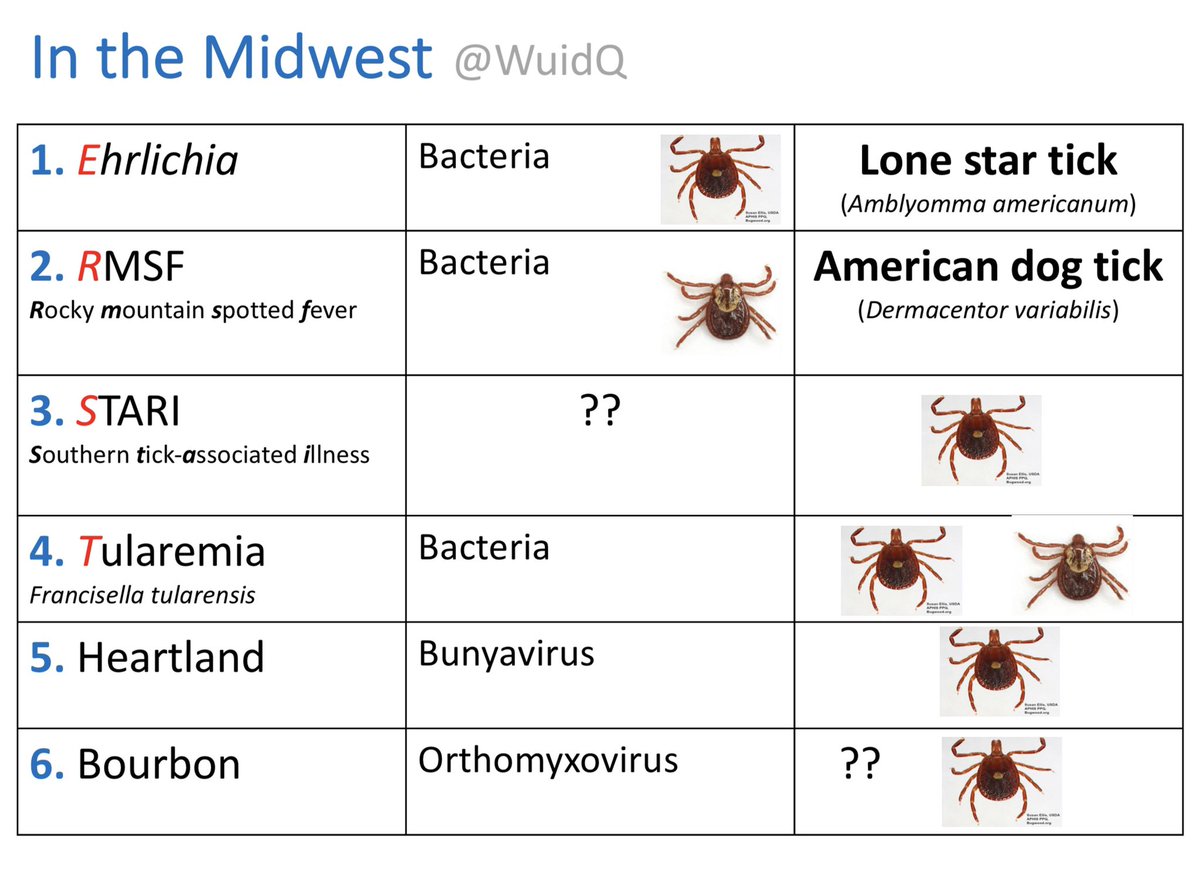

 [Part 2/2] Path Gram/GMS/AFB & Cx (-). 14d Bactrim - no relief. 6 most ago, immigrated to the US from Norway where he was a hunter. Owned livestock, +tick/arthropod bites. Remote h/o treated latent TB. Which of the ff is the most likely cause?
[Part 2/2] Path Gram/GMS/AFB & Cx (-). 14d Bactrim - no relief. 6 most ago, immigrated to the US from Norway where he was a hunter. Owned livestock, +tick/arthropod bites. Remote h/o treated latent TB. Which of the ff is the most likely cause?

 Part 2 of 2
Part 2 of 2
 Part 2/2 case continued..
Part 2/2 case continued..

