ID Miscellany|physical Exam|Signs|Humanities #idmesh
𝙏𝙚𝙢𝙥𝙚𝙧𝙖𝙩𝙪𝙧𝙚-𝙥𝙪𝙡𝙨𝙚 𝙙𝙞𝙨𝙨𝙤𝙘𝙞𝙖𝙩𝙞𝙤𝙣 (𝙁𝙖𝙜𝙚𝙩'𝙨 𝙨𝙞𝙜𝙣)
1/11
For every 1 deg F rise in temp, HR incrementally increases by 8-10 bpm (𝓛𝓲𝓮𝓫𝓮𝓻𝓶𝓮𝓲𝓼𝓽𝓮𝓻’𝓼 𝓻𝓾𝓵𝓮)
academic.oup.com/qjmed/article/…
𝙏𝙚𝙢𝙥𝙚𝙧𝙖𝙩𝙪𝙧𝙚-𝙥𝙪𝙡𝙨𝙚 𝙙𝙞𝙨𝙨𝙤𝙘𝙞𝙖𝙩𝙞𝙤𝙣 (𝙁𝙖𝙜𝙚𝙩'𝙨 𝙨𝙞𝙜𝙣)
1/11
For every 1 deg F rise in temp, HR incrementally increases by 8-10 bpm (𝓛𝓲𝓮𝓫𝓮𝓻𝓶𝓮𝓲𝓼𝓽𝓮𝓻’𝓼 𝓻𝓾𝓵𝓮)
academic.oup.com/qjmed/article/…
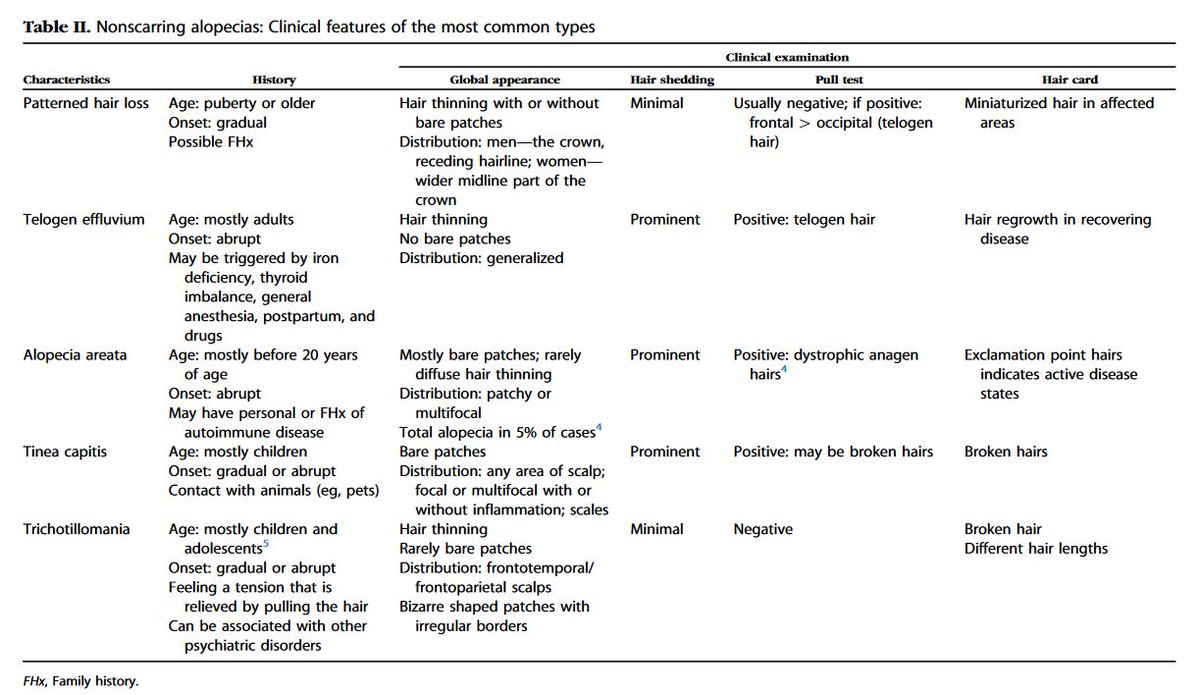
2/11
This is a physical sign that may have become less popular now because of more sophisticated methods of diagnosing infections.
But knowing its application can expand our clinical reasoning toolkit and enhance bedside diagnosis and teaching.
This is a physical sign that may have become less popular now because of more sophisticated methods of diagnosing infections.
But knowing its application can expand our clinical reasoning toolkit and enhance bedside diagnosis and teaching.
3/11
There are a couple of ways to determine whether 𝙏𝙚𝙢𝙥𝙚𝙧𝙖𝙩𝙪𝙧𝙚-𝙥𝙪𝙡𝙨𝙚 𝙙𝙞𝙨𝙨𝙤𝙘𝙞𝙖𝙩𝙞𝙤𝙣 is present.
▪️ using a math equation to derive a cut-off HR below which, a diagnosis of "relative bradycardia" can be made
▪️ applying a set of criteria
There are a couple of ways to determine whether 𝙏𝙚𝙢𝙥𝙚𝙧𝙖𝙩𝙪𝙧𝙚-𝙥𝙪𝙡𝙨𝙚 𝙙𝙞𝙨𝙨𝙤𝙘𝙞𝙖𝙩𝙞𝙤𝙣 is present.
▪️ using a math equation to derive a cut-off HR below which, a diagnosis of "relative bradycardia" can be made
▪️ applying a set of criteria
4/11
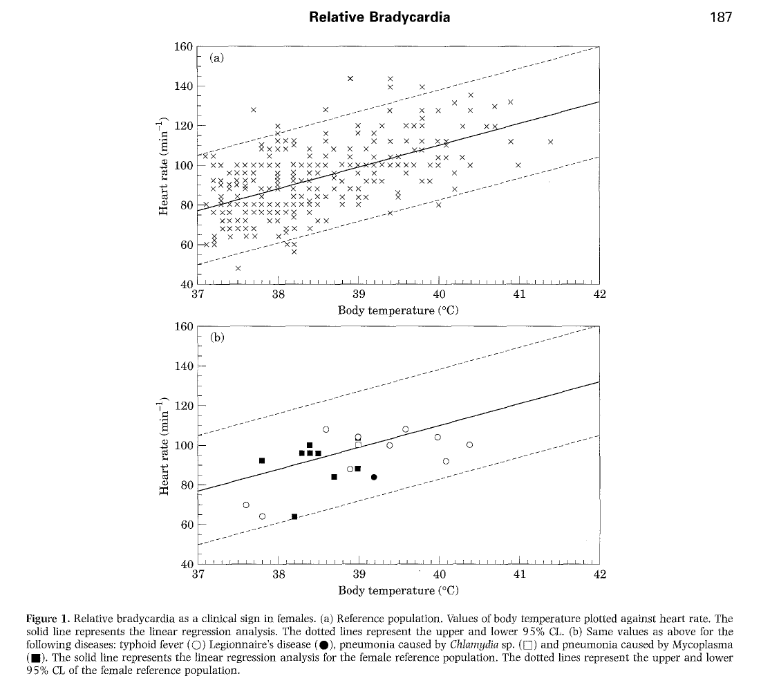
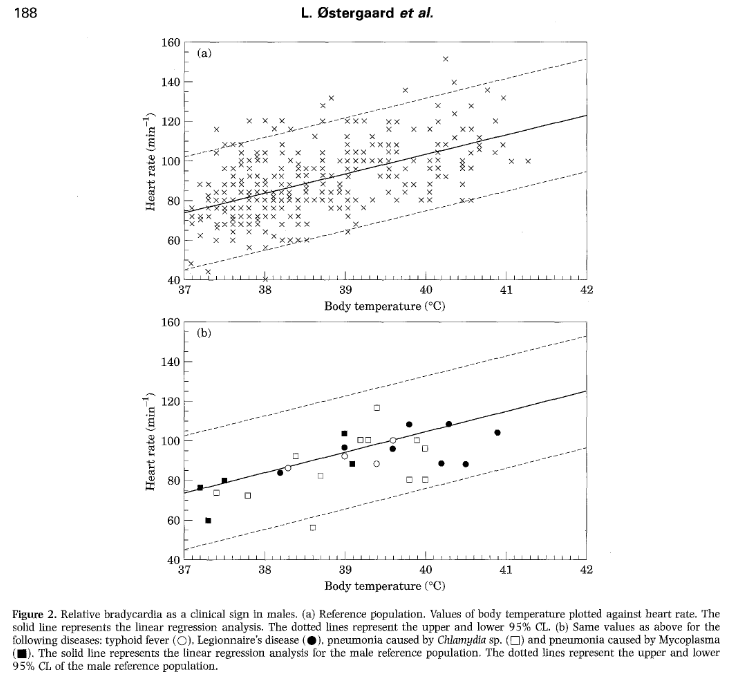
Ostergaard, et al proposed a calculation to determine “relative” bradycardia" -- a pulse rate lower than 95% CI for the patient’s temp (determined among 673 patients 👇):
Men: if HR <10.2 x T0C – 333
Women: if HR <11 x T0C – 359
sciencedirect.com/science/articl…

Ostergaard, et al proposed a calculation to determine “relative” bradycardia" -- a pulse rate lower than 95% CI for the patient’s temp (determined among 673 patients 👇):
Men: if HR <10.2 x T0C – 333
Women: if HR <11 x T0C – 359
sciencedirect.com/science/articl…
5/11
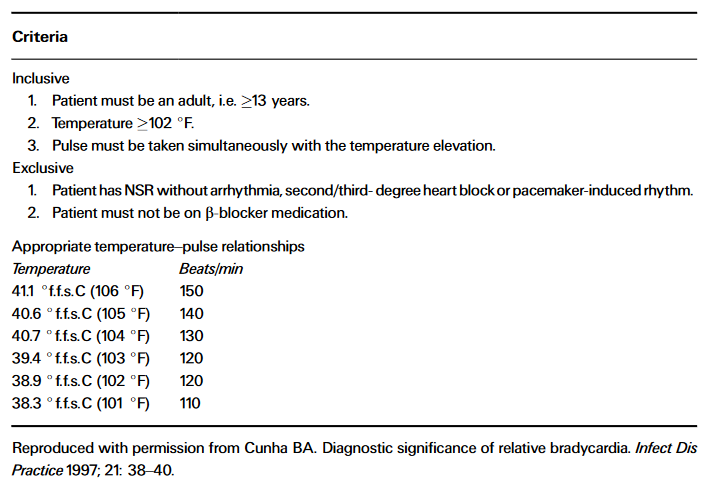
On the other hand, Cunha proposed a more permissive criteria to determine relative bradycardia 👇, based on:
▪️ a set of inclusion/exclusion criteria
▪️ set of expected HRs per given temp
sciencedirect.com/science/articl…
On the other hand, Cunha proposed a more permissive criteria to determine relative bradycardia 👇, based on:
▪️ a set of inclusion/exclusion criteria
▪️ set of expected HRs per given temp
sciencedirect.com/science/articl…
6/11
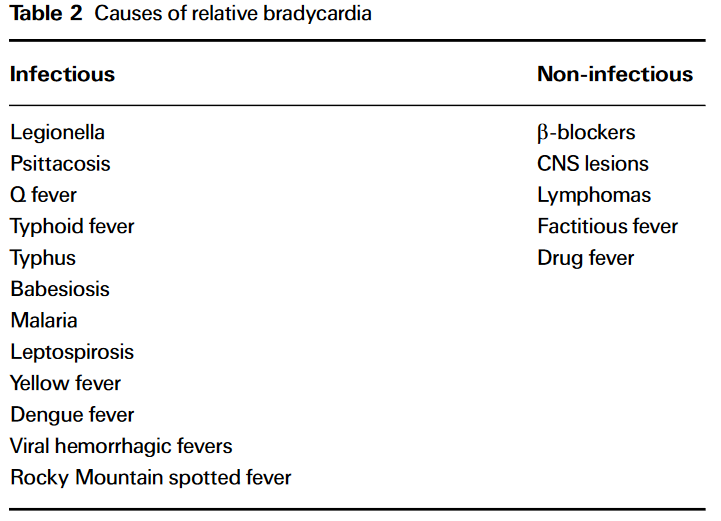
Whatever method you use, once you determine that “relative bradycardia” is present, you can look at a list and be familiar with the many conditions (infectious and non-infectious) that it has been traditionally associated with 👇
sciencedirect.com/science/articl…
Whatever method you use, once you determine that “relative bradycardia” is present, you can look at a list and be familiar with the many conditions (infectious and non-infectious) that it has been traditionally associated with 👇
sciencedirect.com/science/articl…
7/11
The exact sensitivity and specificity of the Faget’s sign is unknown. But data seems to show its diagnostic value in the following infections:
1⃣ Legionella
2⃣ Chlamydia
3⃣ Salmonella typhi (typhoid fever)
4⃣ Dengue
The exact sensitivity and specificity of the Faget’s sign is unknown. But data seems to show its diagnostic value in the following infections:
1⃣ Legionella
2⃣ Chlamydia
3⃣ Salmonella typhi (typhoid fever)
4⃣ Dengue
8/11
Among close to 700 patients, relative bradycardia had no predictive value regarding most likely infection but found only in specific diseases:
▪️ typhoid fever (but NOT non-typhi Salmonella)
▪️ Legionella & Chlamydia pneumonia (but NOT Mycoplasma)
sciencedirect.com/science/articl…
Among close to 700 patients, relative bradycardia had no predictive value regarding most likely infection but found only in specific diseases:
▪️ typhoid fever (but NOT non-typhi Salmonella)
▪️ Legionella & Chlamydia pneumonia (but NOT Mycoplasma)
sciencedirect.com/science/articl…
9/11
Case-control study (N=160) in Japan, the presence of relative bradycardia was diagnostic of typhoid fever (OR 11.7, LR+ 1.72).
journals.plos.org/plosone/articl…
Case-control study (N=160) in Japan, the presence of relative bradycardia was diagnostic of typhoid fever (OR 11.7, LR+ 1.72).
journals.plos.org/plosone/articl…
10/11
Case control study (N=70) in Singapore, relative bradycardia was a significant feature of dengue but not other causes of infection (p < 0.001))
wwwnc.cdc.gov/eid/article/13…
Case control study (N=70) in Singapore, relative bradycardia was a significant feature of dengue but not other causes of infection (p < 0.001))
wwwnc.cdc.gov/eid/article/13…
11/11
So next time you see a febrile patient (e.g. patient coming w/ CAP, returned traveler), try to see if you can apply the 𝙁𝙖𝙜𝙚𝙩'𝙨 𝙨𝙞𝙜𝙣.
Has this sign ever been useful in your practice? Tell us about it. @DocWoc71 @BradCutrellMD @CarlosdelRio7 @PaulSaxMD @TxID_Edu
So next time you see a febrile patient (e.g. patient coming w/ CAP, returned traveler), try to see if you can apply the 𝙁𝙖𝙜𝙚𝙩'𝙨 𝙨𝙞𝙜𝙣.
Has this sign ever been useful in your practice? Tell us about it. @DocWoc71 @BradCutrellMD @CarlosdelRio7 @PaulSaxMD @TxID_Edu
• • •
Missing some Tweet in this thread? You can try to
force a refresh