.@goKDIGO Controversies Conference on Optimal Anemia Management in CKD
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 kdigo.org/wp-content/upl…
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 kdigo.org/wp-content/upl…

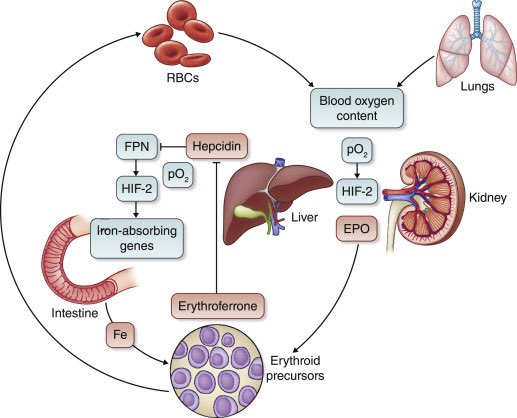
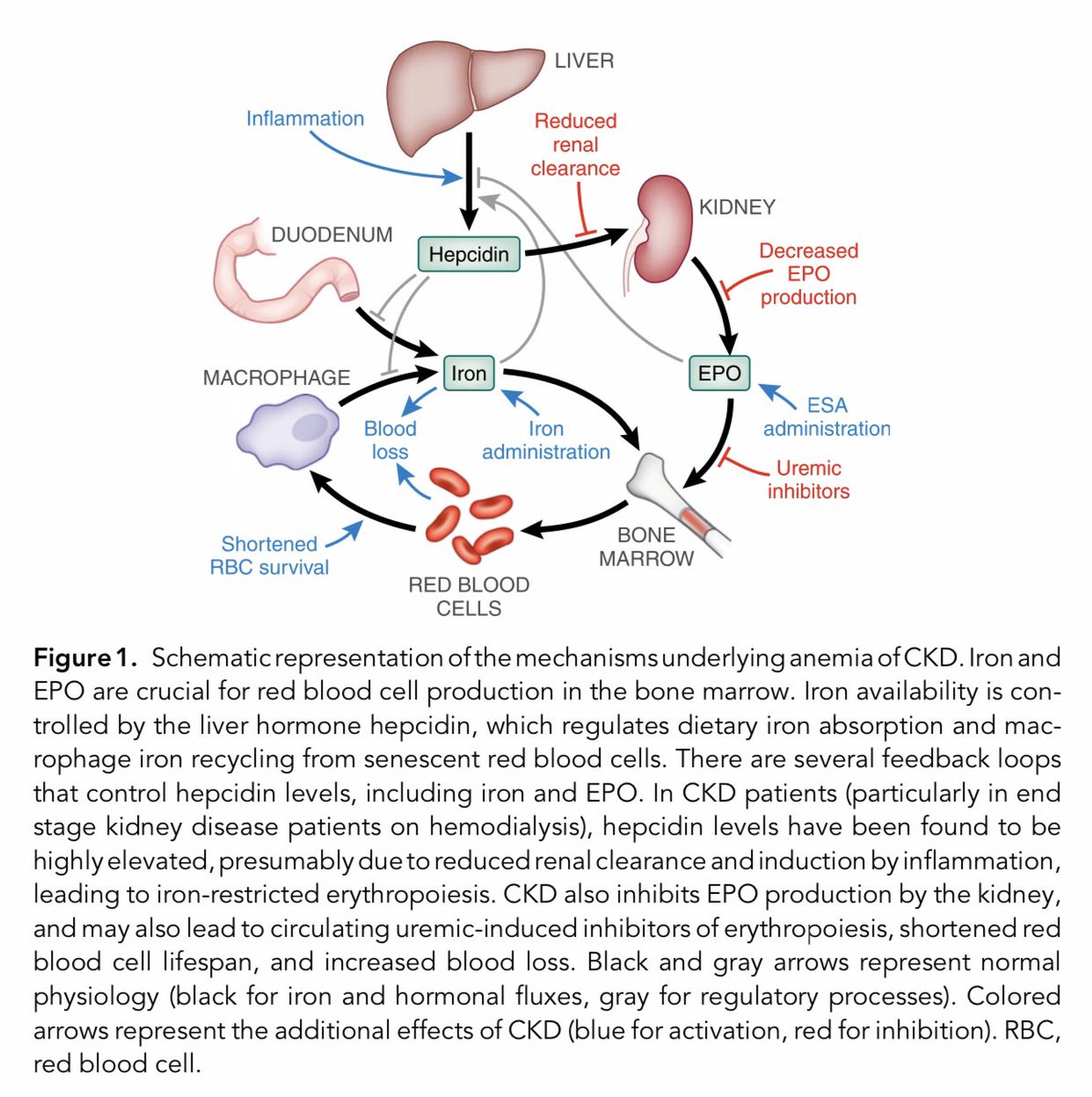
Mechanisms of anemia in CKD ca. 2012 from @JASN_News
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 jasn.asnjournals.org/content/jnephr…

#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 jasn.asnjournals.org/content/jnephr…


Update on Anemia in ESKD and Earlier Stages of CKD: Core Curriculum 2018 from @AJKDonline @sfishbane
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 ajkd.org/article/S0272-…



#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 ajkd.org/article/S0272-…




Potential mechanism of increased CV risk with higher hemoglobin targets in ESA studies
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 ncbi.nlm.nih.gov/pmc/articles/P…

#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 ncbi.nlm.nih.gov/pmc/articles/P…


Hypoxia-inducible factor (HIF) gene targets
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 ncbi.nlm.nih.gov/pmc/articles/P…

#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 ncbi.nlm.nih.gov/pmc/articles/P…


PIVOTAL: Among patients undergoing hemodialysis, a high-dose IV Fe regimen administered proactively was superior to a low-dose regimen administered reactively & resulted in lower doses of ESA being administered from @NEJM
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 nejm.org/doi/pdf/10.105…

#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 nejm.org/doi/pdf/10.105…


Crosstalk between iron and oxygen sensing
📌 HIF-dependent gene expression is iron dependent
📌 Iron-absorbing genes are HIF target genes
📌 FPN stabilizes HIF-2 in enterocytes
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 kidney-international.org/article/S0085-…
📌 HIF-dependent gene expression is iron dependent
📌 Iron-absorbing genes are HIF target genes
📌 FPN stabilizes HIF-2 in enterocytes
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 kidney-international.org/article/S0085-…
Prevalence of anemia of CKD in the US 🇺🇸
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 journals.plos.org/plosone/articl…


#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 journals.plos.org/plosone/articl…



Traditionally used markers of iron status, ⬇️ TSAT, especially TSAT< 10%, is most strongly associated with the risk of adverse outcomes in CKD patients irrespective of serum ferritin level
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 bmcnephrol.biomedcentral.com/track/pdf/10.1…

#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 bmcnephrol.biomedcentral.com/track/pdf/10.1…


Suggested management of reactions to IV iron
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 kdigo.org/wp-content/upl…



#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 kdigo.org/wp-content/upl…




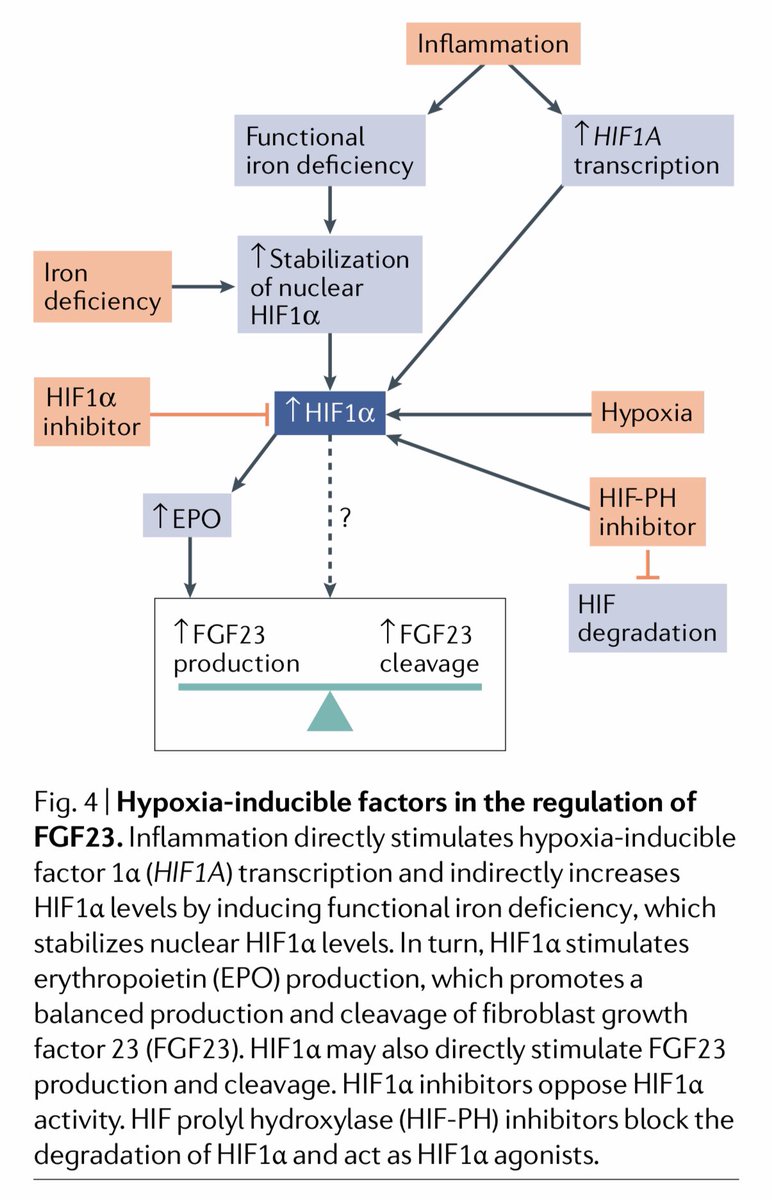
HIF in the regulation of FGF23 ca. 2019 from @NatRevNeph
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 nature.com/articles/s4158…

#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 nature.com/articles/s4158…

Effects of Molidustat in the Treatment of Anemia in CKD ca. 2019 from @CJASN
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 cjasn.asnjournals.org/content/clinja…

#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 cjasn.asnjournals.org/content/clinja…


Daprodustat produced dose-dependent changes in hemoglobin over the first 4 weeks after switching from a stable dose of rhEPO as well as maintained hemoglobin target levels over 24 weeks
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 academic.oup.com/ckj/article/12…

#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 academic.oup.com/ckj/article/12…


Vadadustat, a novel oral HIF stabilizer, provides effective anemia treatment in nondialysis-dependent CKD
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 kidney-international.org/article/S0085-…


#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 kidney-international.org/article/S0085-…



List of Oral Iron Agents Used for Treating Anemia in Patients With CKD ca. 2019
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 ackdjournal.org/article/S1548-…

#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 ackdjournal.org/article/S1548-…


Iron Preparations in the Treatment of Anemia in Non-Dialysis Dependent CKD ca. 2019
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 ackdjournal.org/article/S1548-…


#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 ackdjournal.org/article/S1548-…



Iron Preparations in the Treatment of Anemia in Dialysis Dependent CKD ca. 2019
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 ackdjournal.org/article/S1548-…


#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 ackdjournal.org/article/S1548-…



Pathogenesis of renal anemia and novel and emerging therapies
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 jasn.asnjournals.org/content/jnephr…


#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 jasn.asnjournals.org/content/jnephr…


Diagnostic tests and therapeutic targets 🎯 for anemia of CKD
#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 kdigo.org/wp-content/upl…



#KDIGOAnemia 🇪🇸 #Nephpearls
👉🏼 kdigo.org/wp-content/upl…




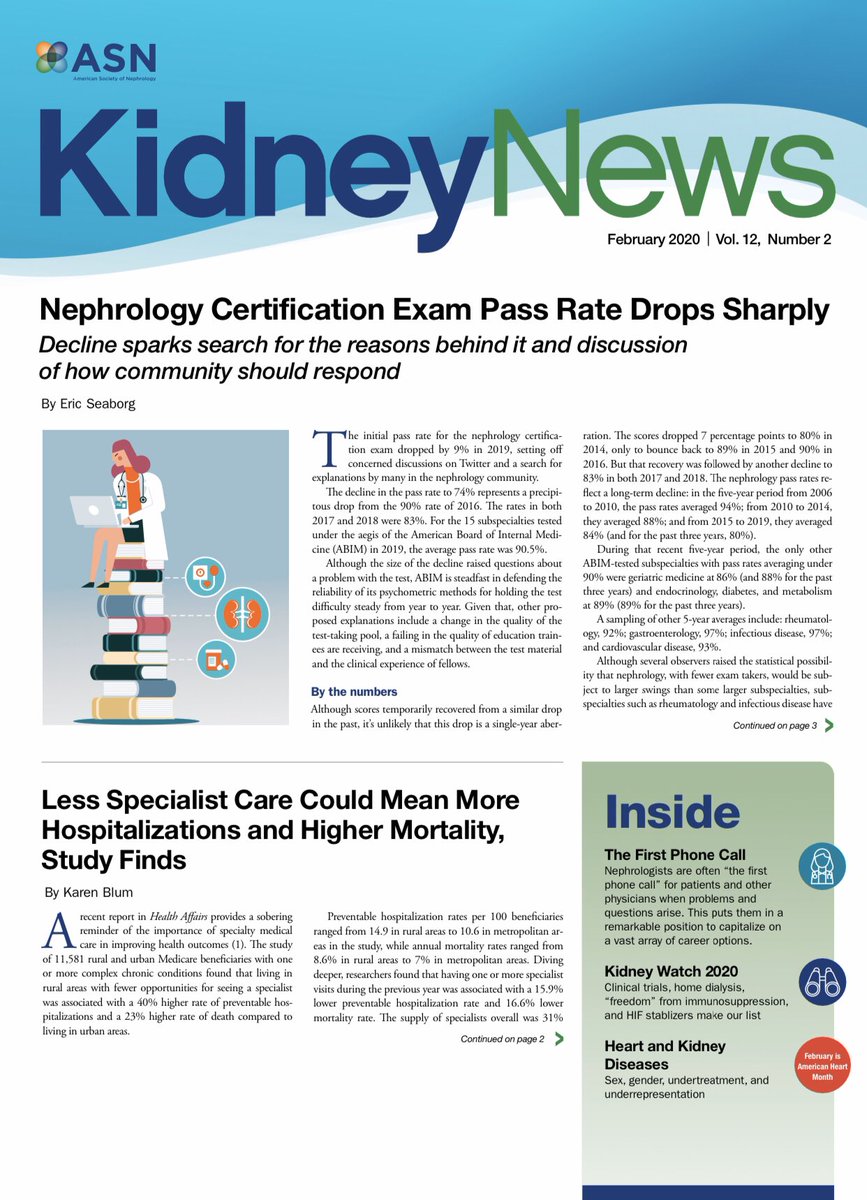
HIF PHD inhibitors in clinical development ca. 2019
#Nephpearls #Welcome2020
👉🏼 asn-online.org/publications/k…

#Nephpearls #Welcome2020
👉🏼 asn-online.org/publications/k…


Check out 👉🏼 Hypoxia-inducible Factor (HIF) Stabilizers for Treating Anemia of CKD
📌 This is my choice for ⚡️Kidney Watch 2020⚡️ published in the February 2020 issue of @KidneyNews
#Nephpearls
👉🏼 asn-online.org/publications/k…


📌 This is my choice for ⚡️Kidney Watch 2020⚡️ published in the February 2020 issue of @KidneyNews
#Nephpearls
👉🏼 asn-online.org/publications/k…


Landmark Trials in Anemia and CKD from @RenalFellowNtwk @xaviervel @landmark_neph #Nephpearls
👉🏼 renalfellow.org/2020/02/19/lan…
👉🏼 renalfellow.org/2020/02/19/lan…

Effect of Ferric Citrate versus Ferrous Sulfate on Iron and Phosphate Parameters in Patients with Iron Deficiency and CKD ca. 2020 from @CJASN #Nephpearls
👉🏼 cjasn.asnjournals.org/content/clinja…



👉🏼 cjasn.asnjournals.org/content/clinja…




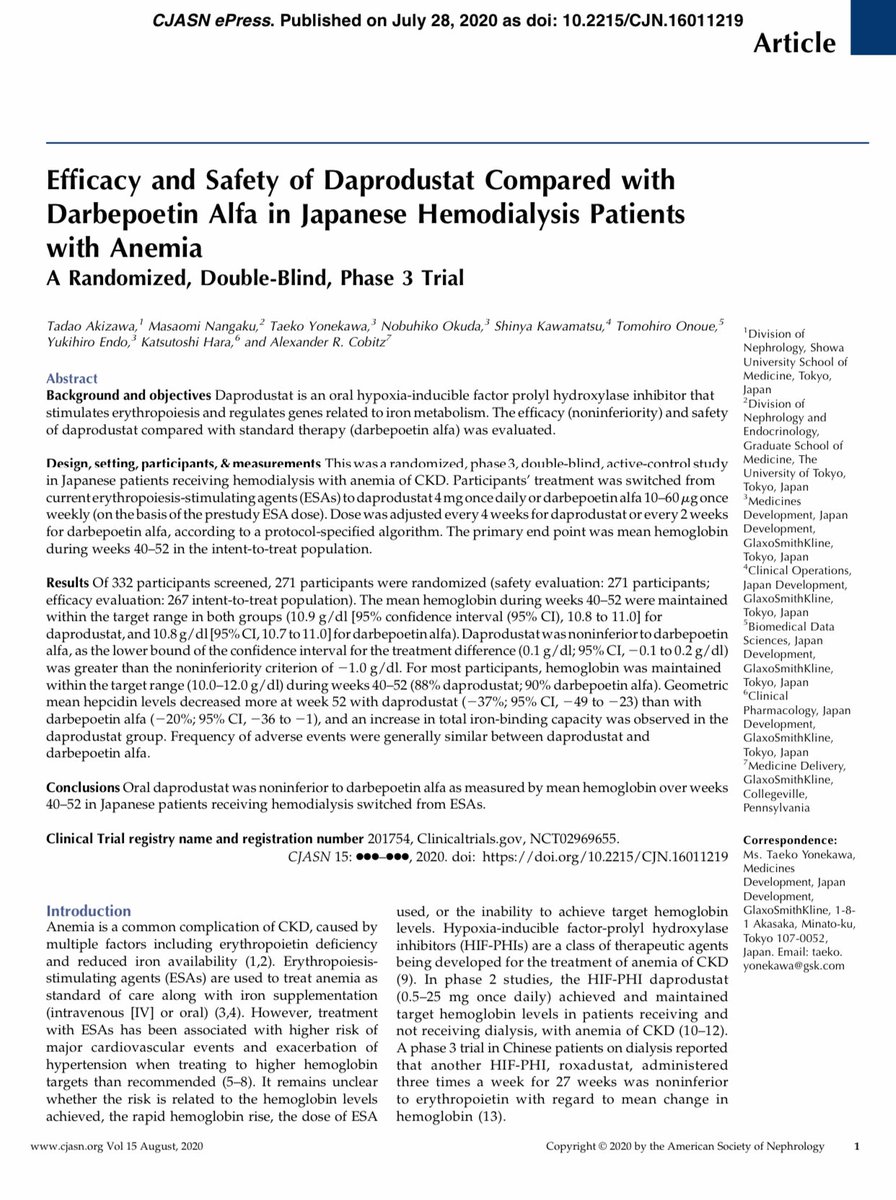
Oral daprodustat was noninferior to darbepoetin alfa as measured by mean hemoglobin over weeks 40–52 in Japanese 🇯🇵 patients receiving hemodialysis switched from ESAs ca. 2020 from @CJASN #Nephpearls
👉🏼 cjasn.asnjournals.org/content/clinja…



👉🏼 cjasn.asnjournals.org/content/clinja…



• • •
Missing some Tweet in this thread? You can try to
force a refresh