ID Miscellany|physical Exam|Signs|Humanities #idmesh
𝐂𝐨𝐧𝐣𝐮𝐧𝐜𝐭𝐢𝐯𝐚𝐥 𝐬𝐮𝐟𝐟𝐮𝐬𝐢𝐨𝐧
1/11
Is an important clue for leptospirosis that may often be overlooked on exam.
Pic from: link.springer.com/chapter/10.100…
𝐂𝐨𝐧𝐣𝐮𝐧𝐜𝐭𝐢𝐯𝐚𝐥 𝐬𝐮𝐟𝐟𝐮𝐬𝐢𝐨𝐧
1/11
Is an important clue for leptospirosis that may often be overlooked on exam.
Pic from: link.springer.com/chapter/10.100…

2/11
What is it?
Simply put, it is a form of non-exudative conjunctivitis
1⃣ Non-exudative:
▪️ No purulent discharge
▪️ No matting of eyes in the morning
What is it?
Simply put, it is a form of non-exudative conjunctivitis
1⃣ Non-exudative:
▪️ No purulent discharge
▪️ No matting of eyes in the morning
3/11
2⃣ Conjunctivitis: means that,
▪️ Pattern of eye redness 👉 red, dilated vessels maximal at the periphery (from the palpebral to the bulbar conjunctivae)
2⃣ Conjunctivitis: means that,
▪️ Pattern of eye redness 👉 red, dilated vessels maximal at the periphery (from the palpebral to the bulbar conjunctivae)

4/11
It is NOT 𝐂𝐨𝐧𝐣𝐮𝐧𝐜𝐭𝐢𝐯𝐚𝐥 𝐬𝐮𝐟𝐟𝐮𝐬𝐢𝐨𝐧 if w/:
▪️ Ciliary flush (redness maximal in the limbus👇) (1)
▪️ Eye pain (2)
▪️ Reduced visual acuity (3)
▪️ Pupillary abnormalities (4)

It is NOT 𝐂𝐨𝐧𝐣𝐮𝐧𝐜𝐭𝐢𝐯𝐚𝐥 𝐬𝐮𝐟𝐟𝐮𝐬𝐢𝐨𝐧 if w/:
▪️ Ciliary flush (redness maximal in the limbus👇) (1)
▪️ Eye pain (2)
▪️ Reduced visual acuity (3)
▪️ Pupillary abnormalities (4)


5/11
Presence of above, 𝘪𝘯𝘴𝘵𝘦𝘢𝘥, would suggest (#'s refer to designation from above list):
▪️ Iritis (1, 2, 3, 4-constricted pupil/poor response)
▪️ Keratitis (1, 2, 3, hazy cornea)
▪️ Scleritis (2 – deep pain, ocular tenderness)
Lots of ID & non-ID DDX for above.
Presence of above, 𝘪𝘯𝘴𝘵𝘦𝘢𝘥, would suggest (#'s refer to designation from above list):
▪️ Iritis (1, 2, 3, 4-constricted pupil/poor response)
▪️ Keratitis (1, 2, 3, hazy cornea)
▪️ Scleritis (2 – deep pain, ocular tenderness)
Lots of ID & non-ID DDX for above.
6/11
𝐂𝐨𝐧𝐣𝐮𝐧𝐜𝐭𝐢𝐯𝐚𝐥 𝐬𝐮𝐟𝐟𝐮𝐬𝐢𝐨𝐧 is “one of the most reliable and distinguishing features of leptospirosis” (UpToDate).
When you do an online search for "𝐂𝐨𝐧𝐣𝐮𝐧𝐜𝐭𝐢𝐯𝐚𝐥 𝐬𝐮𝐟𝐟𝐮𝐬𝐢𝐨𝐧", 99% of the time, you will get “leptospirosis”.
𝐂𝐨𝐧𝐣𝐮𝐧𝐜𝐭𝐢𝐯𝐚𝐥 𝐬𝐮𝐟𝐟𝐮𝐬𝐢𝐨𝐧 is “one of the most reliable and distinguishing features of leptospirosis” (UpToDate).
When you do an online search for "𝐂𝐨𝐧𝐣𝐮𝐧𝐜𝐭𝐢𝐯𝐚𝐥 𝐬𝐮𝐟𝐟𝐮𝐬𝐢𝐨𝐧", 99% of the time, you will get “leptospirosis”.
7/11
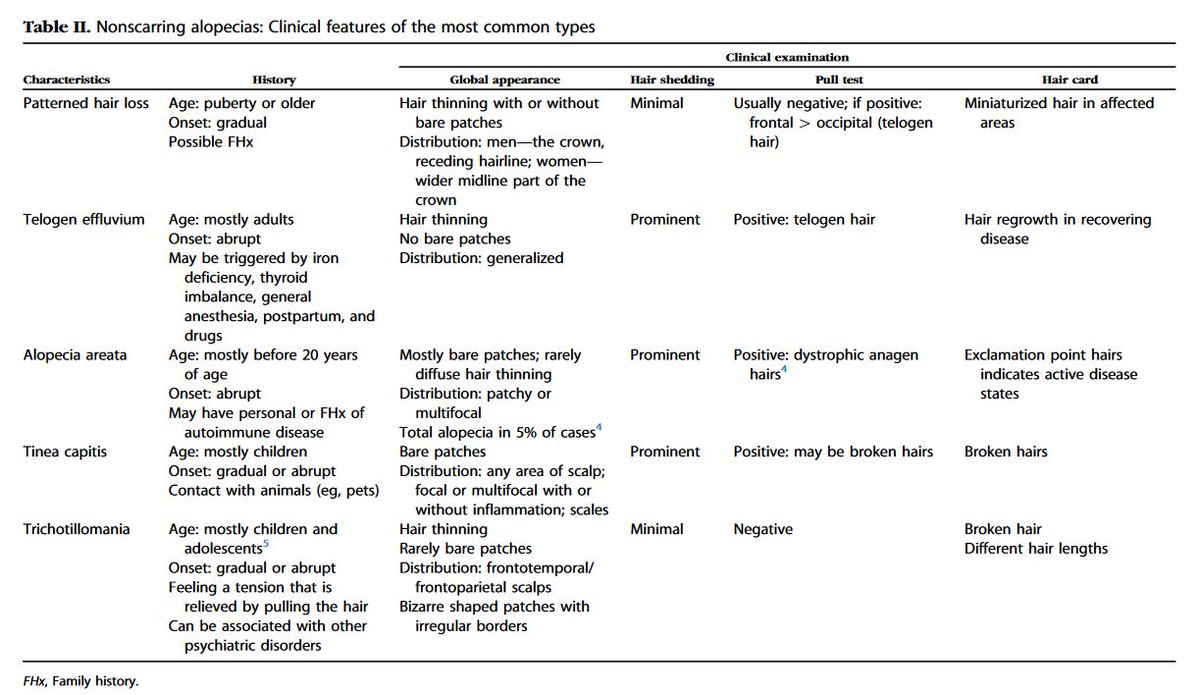
But when you look for DDX of non-exudative conjunctivitis (especially bilateral), you’ll see that it can also be seen in a variety of conditions.
But when you look for DDX of non-exudative conjunctivitis (especially bilateral), you’ll see that it can also be seen in a variety of conditions.
8/11
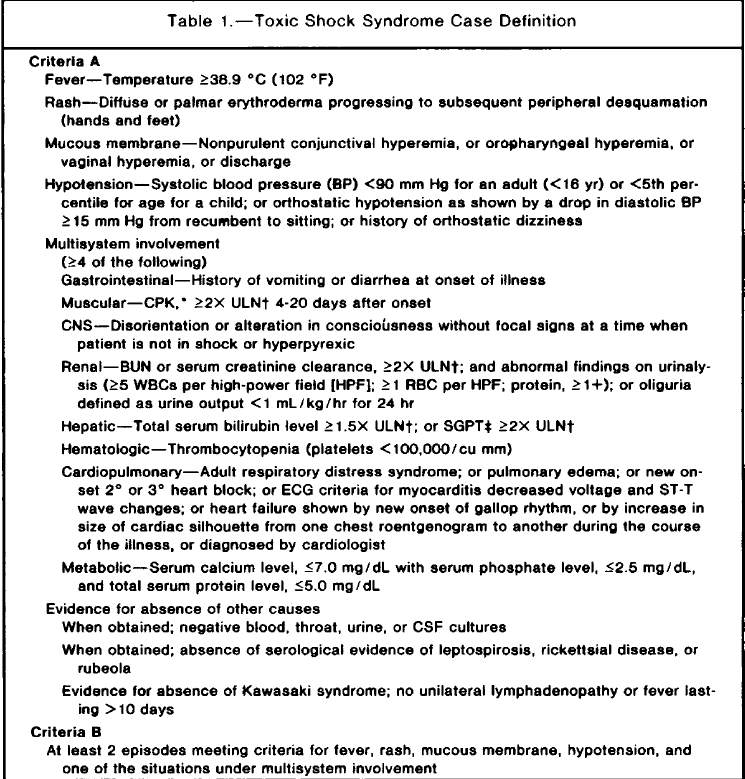
Differential diagnoses of B/L non-exudative conjunctivitis:
▪️ Viral, esp adenovirus & measles
▪️ RMSF (rarely) cdc.gov/mmwr/volumes/6…
▪️ Kawasaki👇 link.springer.com/article/10.100…
▪️ Toxic shock syndrome👇 jamanetwork.com/journals/jama/…

Differential diagnoses of B/L non-exudative conjunctivitis:
▪️ Viral, esp adenovirus & measles
▪️ RMSF (rarely) cdc.gov/mmwr/volumes/6…
▪️ Kawasaki👇 link.springer.com/article/10.100…
▪️ Toxic shock syndrome👇 jamanetwork.com/journals/jama/…

9/11
But (+) 𝐂𝐨𝐧𝐣𝐮𝐧𝐜𝐭𝐢𝐯𝐚𝐥 𝐬𝐮𝐟𝐟𝐮𝐬𝐢𝐨𝐧 in a patient w/ 𝘯𝘰𝘯𝘴𝘱𝘦𝘤𝘪𝘧𝘪𝘤 fever, in the right epidemiologic setting, should raise suspicion for leptospirosis.
👉 Especially during the septicemic phase where SSX can be 𝘯𝘰𝘯𝘴𝘱𝘦𝘤𝘪𝘧𝘪𝘤
But (+) 𝐂𝐨𝐧𝐣𝐮𝐧𝐜𝐭𝐢𝐯𝐚𝐥 𝐬𝐮𝐟𝐟𝐮𝐬𝐢𝐨𝐧 in a patient w/ 𝘯𝘰𝘯𝘴𝘱𝘦𝘤𝘪𝘧𝘪𝘤 fever, in the right epidemiologic setting, should raise suspicion for leptospirosis.
👉 Especially during the septicemic phase where SSX can be 𝘯𝘰𝘯𝘴𝘱𝘦𝘤𝘪𝘧𝘪𝘤

10/11
"Red eye" in ID is a helpful clue to a variety of conditions (ID & non-ID). At the 𝘮𝘪𝘯𝘪𝘮𝘶𝘮, should examine:
▪️ Pattern of redness, vision, cornea, pain, pupils (direct/indirect, convergence)
As detailed above, can enrich clinical reasoning & form illness scripts!
"Red eye" in ID is a helpful clue to a variety of conditions (ID & non-ID). At the 𝘮𝘪𝘯𝘪𝘮𝘶𝘮, should examine:
▪️ Pattern of redness, vision, cornea, pain, pupils (direct/indirect, convergence)
As detailed above, can enrich clinical reasoning & form illness scripts!
11/11
In your practice, how often have you seen 𝐂𝐨𝐧𝐣𝐮𝐧𝐜𝐭𝐢𝐯𝐚𝐥 𝐬𝐮𝐟𝐟𝐮𝐬𝐢𝐨𝐧? @DocWoc71 @CarlosdelRio7 @FungalDoc
@TxID_Edu @GermHunterMD @FranciscoMarty_ @cmejiachew @Vaccinologist @EdselSalvana
In your practice, how often have you seen 𝐂𝐨𝐧𝐣𝐮𝐧𝐜𝐭𝐢𝐯𝐚𝐥 𝐬𝐮𝐟𝐟𝐮𝐬𝐢𝐨𝐧? @DocWoc71 @CarlosdelRio7 @FungalDoc
@TxID_Edu @GermHunterMD @FranciscoMarty_ @cmejiachew @Vaccinologist @EdselSalvana
@DocWoc71 @CarlosdelRio7 @FungalDoc @TxID_Edu @GermHunterMD @FranciscoMarty_ @cmejiachew @Vaccinologist @EdselSalvana 11/11 extra 1⃣
Thank you for all your responses. About 40% has not seen conjunctival suffusion.
How common is it? As high as 99%!! See Table 👇 from cmr.asm.org/content/14/2/2…
What other SSX are common? Myalgia, as high as 100%! Headache, as high as 90%.
Thank you for all your responses. About 40% has not seen conjunctival suffusion.
How common is it? As high as 99%!! See Table 👇 from cmr.asm.org/content/14/2/2…
What other SSX are common? Myalgia, as high as 100%! Headache, as high as 90%.

11/11 extra 2⃣
In 1982, WHO introduced a criteria for leptospirosis dx in resource-limited settings (known as the 𝙁𝙖𝙞𝙣𝙚'𝙨 𝙘𝙧𝙞𝙩𝙚𝙧𝙞𝙖).
This has since been modified in 2013 (Sn 95%). 👇 apps.who.int/iris/bitstream…
ncbi.nlm.nih.gov/pmc/articles/P…
In 1982, WHO introduced a criteria for leptospirosis dx in resource-limited settings (known as the 𝙁𝙖𝙞𝙣𝙚'𝙨 𝙘𝙧𝙞𝙩𝙚𝙧𝙞𝙖).
This has since been modified in 2013 (Sn 95%). 👇 apps.who.int/iris/bitstream…
ncbi.nlm.nih.gov/pmc/articles/P…

11/11 extra 3⃣
When I was training in the Philippines, where frequent outbreaks of leptospirosis occurs especially after a flood, we used the Faine's criteria.
It demonstrates the value of conjunctival suffusion & myalgia (esp of the calves) in suspecting leptospirosis.
When I was training in the Philippines, where frequent outbreaks of leptospirosis occurs especially after a flood, we used the Faine's criteria.
It demonstrates the value of conjunctival suffusion & myalgia (esp of the calves) in suspecting leptospirosis.
11/11 extra 4⃣
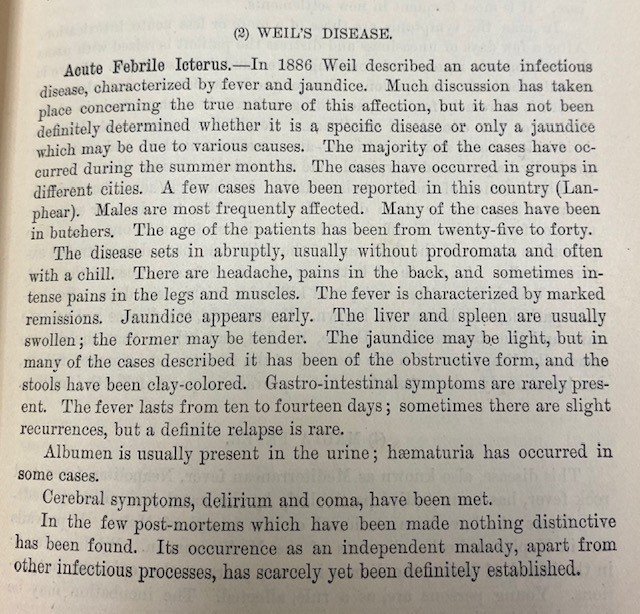
Look what Osler has to say about leptospirosis, in his first edition of Principles and Practice of Medicine (1st edition, 1892)!
At that time, it was a diagnosis of uncertain etiology, as originally described by Weil in 1886. @AdamRodmanMD @BedsideRounds

Look what Osler has to say about leptospirosis, in his first edition of Principles and Practice of Medicine (1st edition, 1892)!
At that time, it was a diagnosis of uncertain etiology, as originally described by Weil in 1886. @AdamRodmanMD @BedsideRounds

• • •
Missing some Tweet in this thread? You can try to
force a refresh