#idgrandrounds
(Part 1 of 2)
31M carpenter from the Midwest, +3 wks b/l blurred vision/eye redness. No pain/discharge, floaters, (+)photophobia/hearing impairment. No headache, fever, N/V. Found to have new HIV dx (CD4 520 VL 120K). Exam: b/l red eyes, nonfocal neuro, no rash.
(Part 1 of 2)
31M carpenter from the Midwest, +3 wks b/l blurred vision/eye redness. No pain/discharge, floaters, (+)photophobia/hearing impairment. No headache, fever, N/V. Found to have new HIV dx (CD4 520 VL 120K). Exam: b/l red eyes, nonfocal neuro, no rash.
#idgrandrounds
(Part 2 of 2)
(-)RPR/TSPOT. N/l CBC/CMP. Optho: +uveitis.
(-)PMH/illicits. MSM. No h/o travel/pets. Brief h/o homelessness but no h/o incarceration.
Differential dx? @CPSolvers @TxID_Edu @jdcooperid @BradCutrellMD @Cortes_Penfield @MohitHarshMD @serotavirus
(Part 2 of 2)
(-)RPR/TSPOT. N/l CBC/CMP. Optho: +uveitis.
(-)PMH/illicits. MSM. No h/o travel/pets. Brief h/o homelessness but no h/o incarceration.
Differential dx? @CPSolvers @TxID_Edu @jdcooperid @BradCutrellMD @Cortes_Penfield @MohitHarshMD @serotavirus
@CPSolvers @TxID_Edu @jdcooperid @BradCutrellMD @Cortes_Penfield @MohitHarshMD @serotavirus #idgrandrounds
1/11
𝐏𝐑𝐎𝐙𝐎𝐍𝐄 was suspected. Diluted sample showed RPR to be 1:1024.
LP was performed and showed evidence of lymphocytic pleocytosis and with a +VDRL.
CASE RESOLUTION: Neuro-ocular syphilis, w/ prozone reaction
1/11
𝐏𝐑𝐎𝐙𝐎𝐍𝐄 was suspected. Diluted sample showed RPR to be 1:1024.
LP was performed and showed evidence of lymphocytic pleocytosis and with a +VDRL.
CASE RESOLUTION: Neuro-ocular syphilis, w/ prozone reaction
2/11
This case highlights the importance maintaining a high index of suspicion for syphilis and the prozone reaction.
𝐏𝐑𝐎𝐙𝐎𝐍𝐄 reaction
1⃣ Causes false negative RPR due to high Ab titers that prevent Ab/Ag lattice formation and agglutination👇 bit.ly/31sEoBI

This case highlights the importance maintaining a high index of suspicion for syphilis and the prozone reaction.
𝐏𝐑𝐎𝐙𝐎𝐍𝐄 reaction
1⃣ Causes false negative RPR due to high Ab titers that prevent Ab/Ag lattice formation and agglutination👇 bit.ly/31sEoBI


3/11
2⃣ Suspect 𝐏𝐑𝐎𝐙𝐎𝐍𝐄 if clinical syndrome is compatible w/ syphilis but RPR is negative (note that in primary syphilis, RPR can be negative and dx is clinical or established by dark field examination). If prozone is suspected, discuss with lab to dilute specimen
2⃣ Suspect 𝐏𝐑𝐎𝐙𝐎𝐍𝐄 if clinical syndrome is compatible w/ syphilis but RPR is negative (note that in primary syphilis, RPR can be negative and dx is clinical or established by dark field examination). If prozone is suspected, discuss with lab to dilute specimen
4/11
3⃣ Generally rare (0.2-3%). Maybe more common in people with HIV bit.ly/31sEoBI.
4⃣ Other risk factors: pregnancy and neurosyphilis 👇. Classically a/w secondary syphilis but can be found in all stages 👇 bit.ly/375eogW
3⃣ Generally rare (0.2-3%). Maybe more common in people with HIV bit.ly/31sEoBI.
4⃣ Other risk factors: pregnancy and neurosyphilis 👇. Classically a/w secondary syphilis but can be found in all stages 👇 bit.ly/375eogW

5/11
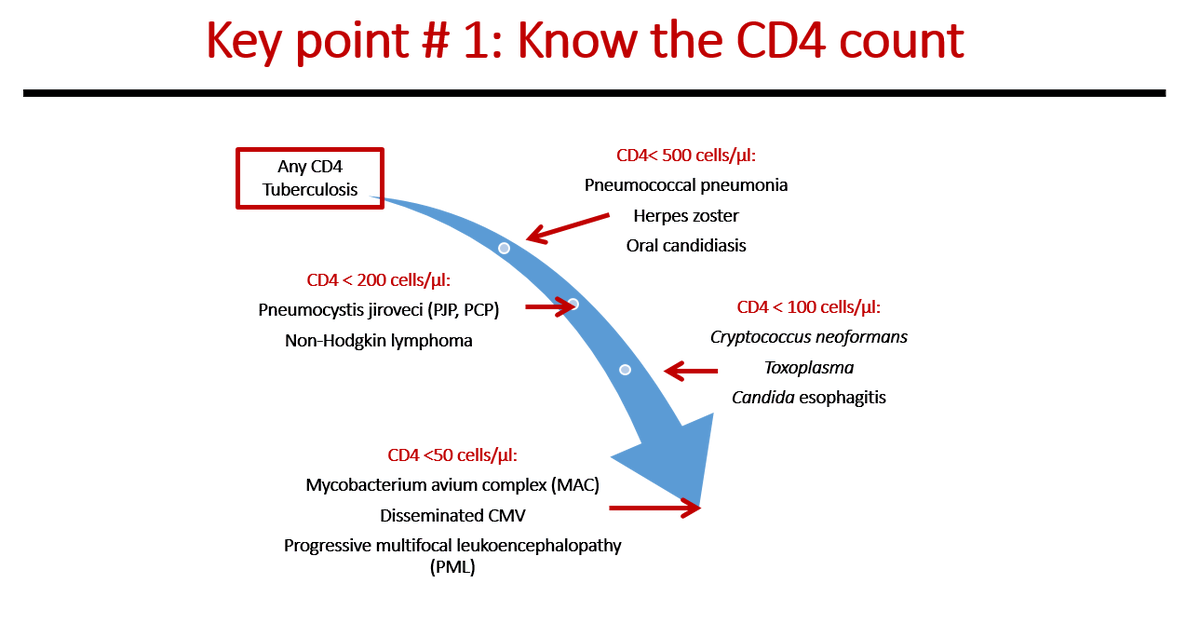
This case also teaches a systematic approach to opportunistic infections in people with HIV.
Step 1⃣ Know the CD4 count. This will give you an idea of the over-all risk of your patient for certain opportunistic infections. 👇
This case also teaches a systematic approach to opportunistic infections in people with HIV.
Step 1⃣ Know the CD4 count. This will give you an idea of the over-all risk of your patient for certain opportunistic infections. 👇
6/11
Step 2⃣ Understand the mechanism behind certain opportunistic infections. This will expand your differential diagnosis and allow you to build an illness script. 👇
Step 2⃣ Understand the mechanism behind certain opportunistic infections. This will expand your differential diagnosis and allow you to build an illness script. 👇

7/11
Step 3⃣ Apply a syndromic approach, guided by the CD4 count & the mechanism of OI. 👇 This one is the hardest step as it requires familiarity with the MANY manifestations (rare & common) of different kinds of infections.
Step 3⃣ Apply a syndromic approach, guided by the CD4 count & the mechanism of OI. 👇 This one is the hardest step as it requires familiarity with the MANY manifestations (rare & common) of different kinds of infections.

8/11
The ⬆️ CD4 count in our patient makes CMV, HSV/VZV (causing progressive outer retinal necrosis or acute retinal necrosis), Toxoplasma unlikely. The combination of ocular (especially uveitis) & otologic findings (in the absence of other CNS signs) speaks highly of syphilis.
The ⬆️ CD4 count in our patient makes CMV, HSV/VZV (causing progressive outer retinal necrosis or acute retinal necrosis), Toxoplasma unlikely. The combination of ocular (especially uveitis) & otologic findings (in the absence of other CNS signs) speaks highly of syphilis.
9/11
I refer you to @Darcy_ID_doc amazing chart on the many causes of ocular disease in people with HIV. Thank you @TxID_Edu for sharing this.
I refer you to @Darcy_ID_doc amazing chart on the many causes of ocular disease in people with HIV. Thank you @TxID_Edu for sharing this.
https://twitter.com/Darcy_ID_doc/status/1203395736278142976?s=20
10/11
For a general approach to a patient w/ red eyes, click 👇 to link you to a previous discussion on #idmesh
For a general approach to a patient w/ red eyes, click 👇 to link you to a previous discussion on #idmesh
https://twitter.com/WuidQ/status/1207386422845554688?s=20
11/11
Many thanks to everyone who participated. @VarunPhadke2 and @ShannonTurvey immediately suspected a prozone reaction! Great job!
Many thanks especially to @hrenoID and @NNolanMD. Case was modified to protect PHIs.
Many thanks to everyone who participated. @VarunPhadke2 and @ShannonTurvey immediately suspected a prozone reaction! Great job!
Many thanks especially to @hrenoID and @NNolanMD. Case was modified to protect PHIs.
7/11 extra
Sharing @BradCutrellMD's AMAZING chart: syndromic approach to OI in HIV 👇.
Taken from CH 39 of our book @FungalDoc @MDdreamchaser @Courtcita @bugdocdavies
👉 Spec A, Escota G, Chrisler C, Davies B, 1ed. Comprehensive Review of Infectious Diseases. Elsevier 2020.
Sharing @BradCutrellMD's AMAZING chart: syndromic approach to OI in HIV 👇.
Taken from CH 39 of our book @FungalDoc @MDdreamchaser @Courtcita @bugdocdavies
👉 Spec A, Escota G, Chrisler C, Davies B, 1ed. Comprehensive Review of Infectious Diseases. Elsevier 2020.

• • •
Missing some Tweet in this thread? You can try to
force a refresh