Concept 1:
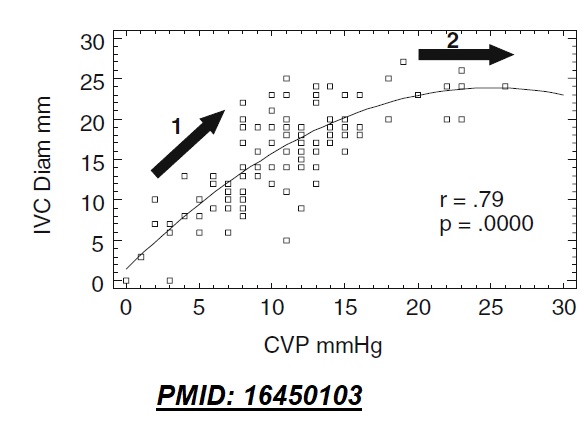
The core mechanism of respirophasic alterations of IVC diameter is its relationship with (actual, not transmural) CVP.
⬇️CVP -->⬆️venous return -->⬇️pressure within the IVC --> tendency to collapse (& vice versa).
Concept 2:
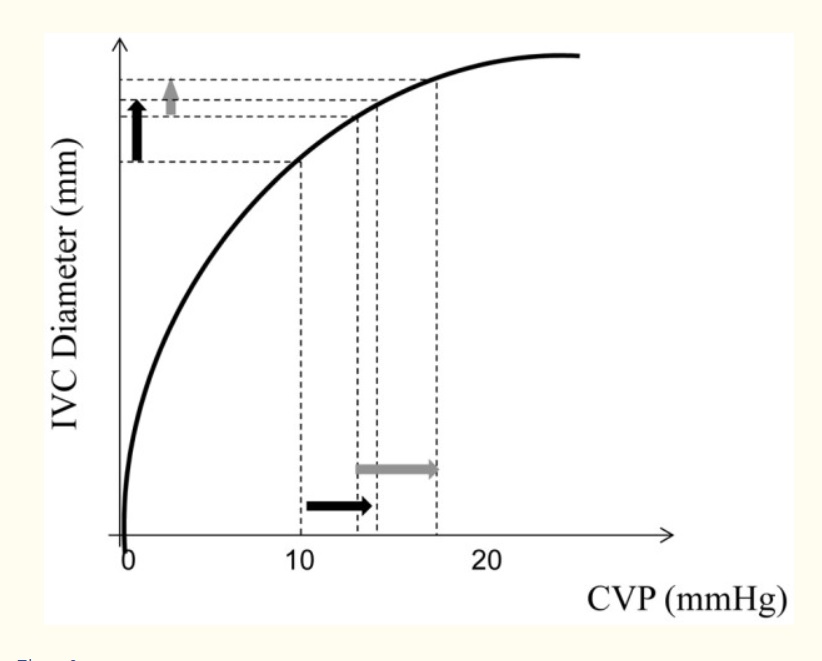
The IVC pressure-diameter relationship
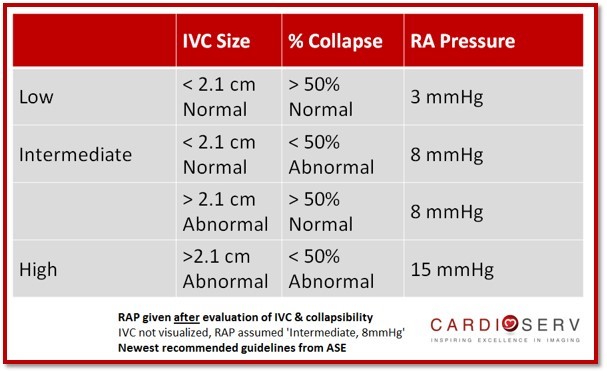
##IVC evaluation in a spontaneously breathing patient -
Inspiration --> ⬇️ITP --> ⬇️CVP --> ⬇️IVC diameter (IVC collapses)
Say CVP reduces by 5 mmHg upon inspiration. Note that the effect on IVC diameter (collapsibility) would be much greater if baseline CVP is lower.
##IVC evaluation in a passive MV patient-
In passive PPV (i.e. no patient efforts e.g. paralyzed):
Inspiration --> ⬆️ITP --> ⬆️CVP --> ⬆️IVC diameter (IVC distends)
Again, the degree of IVC distension will depend on the CVP that would affect how full it is at baseline.
Curiously, as opposed to IVC collapsibility (in NPV), IVC distensibility (in PPV) has NOT shown good correlation with baseline CVP (but very limited data: PMID: 1466886)
However, IVC distensibility HAS shown to predict fluid responsiveness in highly standardized conditions:
These include (i)Passive PPV (ii)TV - 8-12 cc/kg (iii)No cor pulmonale
A distensible IVC is interpreted as evidence of "preload reserve"
But note these are all indirect predictors of fluid responsiveness & in my mind, inferior in principle to direct predictors such as PLR
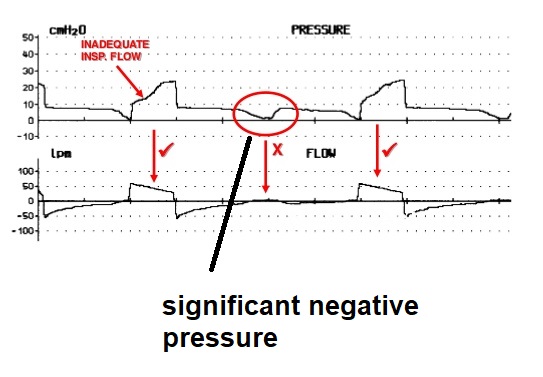
##IVC evaluation in patient-triggered PPV -
This scenario is much more common and rather complex. Patients often have alternating patient-triggered and machine-triggered breaths..
In a patient-triggered breath, there is an initial dip in ITP as the patient triggers.
This includes⬆️abdominal pressure with PPV (see Jon Emile's articles on PulmCCM)
Summary -
-NPV: IVC collapsibility is most helpful in estimating CVP
-Passive PPV: IVC distensibility can predict FR
-Patient-triggered PPV - IVC may collapse but use caution in interpreting.