
Intensivist at UCSF Fresno. Resuscitationist. Sonophile.
#ICUphysiology #Hemodynamics #ECLS #AirwayTwitter #RespiratoryMechanics #ECG #VentRounds
How to get URL link on X (Twitter) App


https://twitter.com/Thind888/status/1752432498041294871Since flow is constant, this 'resistive pressure' remains constant throughout the breath as revealed by the post-inspiratory pause (image 1)



https://twitter.com/Thind888/status/1710769441741631974The main objective was to do a primer on respiratory mechanics and understand how the information obtained from the esophageal balloon can be useful.





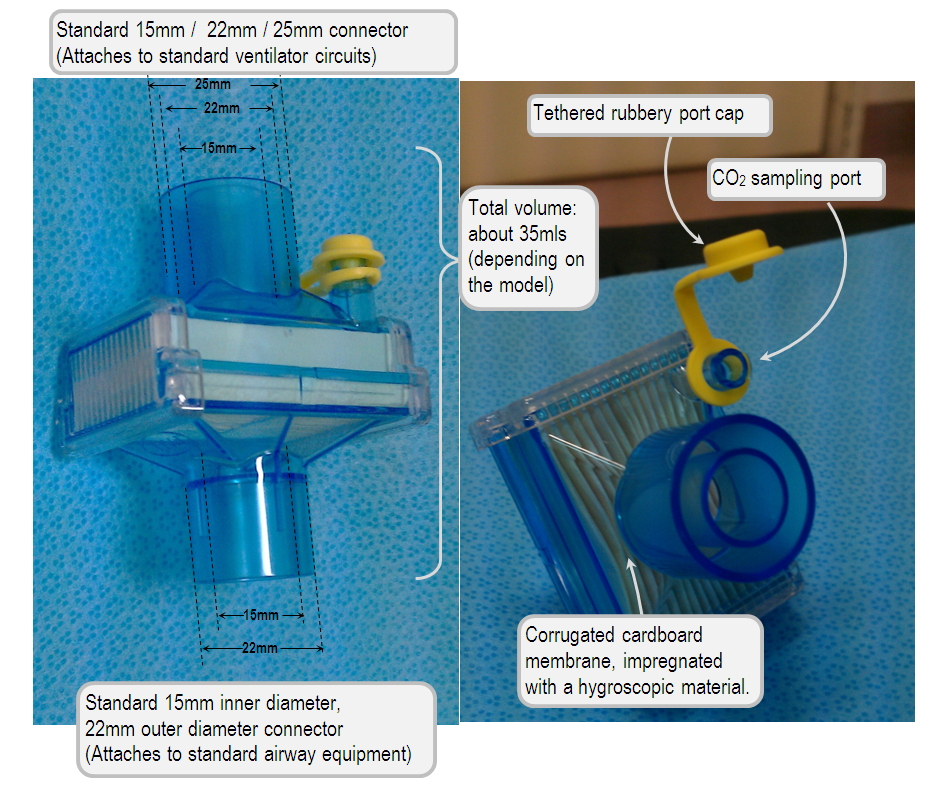
https://twitter.com/rbarbosa91/status/1532622531558903808..In this case, the 'gauge' refers to the luminal diameter (image 1),


 @cjosephy @icmteaching @vaszochios @msiuba @IM_Crit_ @emireles_c @MegriMohammed @HamiltonMedical @ecgoligher @drhaty When we're trying to assess lung stress, what we really want to determine is 'transalveolar pressure'.
@cjosephy @icmteaching @vaszochios @msiuba @IM_Crit_ @emireles_c @MegriMohammed @HamiltonMedical @ecgoligher @drhaty When we're trying to assess lung stress, what we really want to determine is 'transalveolar pressure'.
 2/
2/
https://twitter.com/emily_fri/status/1327695873837502464
 2/
2/
https://twitter.com/load_dependent/status/13076645743852052492/

https://twitter.com/MegriMohammed/status/1291051792155910145Poll:

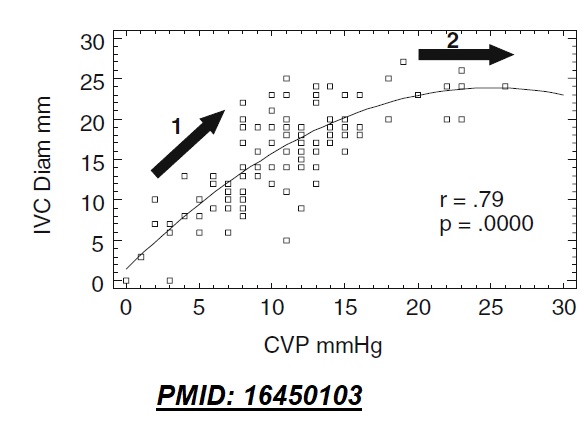
https://twitter.com/Thind888/status/12795643999847997452/ Therefore, the best way to assess tendency for pulmonary congestion is to measure PCWP when ITP is close to zero (at end-expiration), or normalize PCWP for ITP (PCWP – Ppl).






 Compared to baseline, estimated LV preload near the end of the maneuver is ...
Compared to baseline, estimated LV preload near the end of the maneuver is ...

https://twitter.com/ArgaizR/status/1254838818412335106


https://twitter.com/PulmCrit/status/12152475507076177932/ This is perhaps why *conventional* maximum doses of bumetenide are twice as potent (e.g. 2mg/hour of bumetenide vs. 40mg/hour of lasix). So the loop diuretic dosage can be maximized with lower potential for ototoxicity.
https://twitter.com/Thind888/status/1208928426301755392

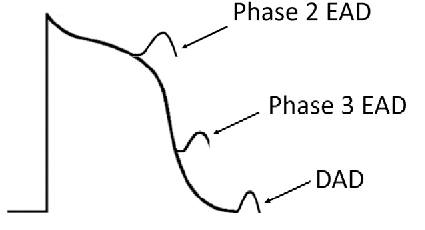
 2/ Scrolling back a few minutes, the following progression is noted (all images are timed).
2/ Scrolling back a few minutes, the following progression is noted (all images are timed).
