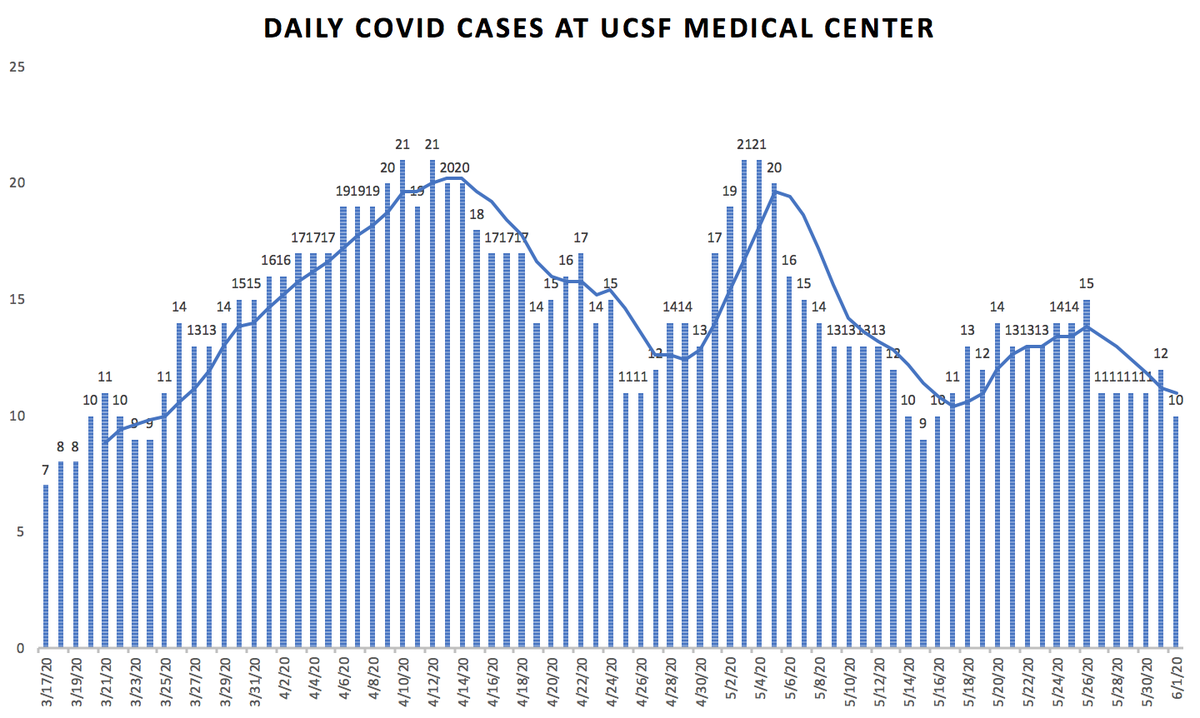
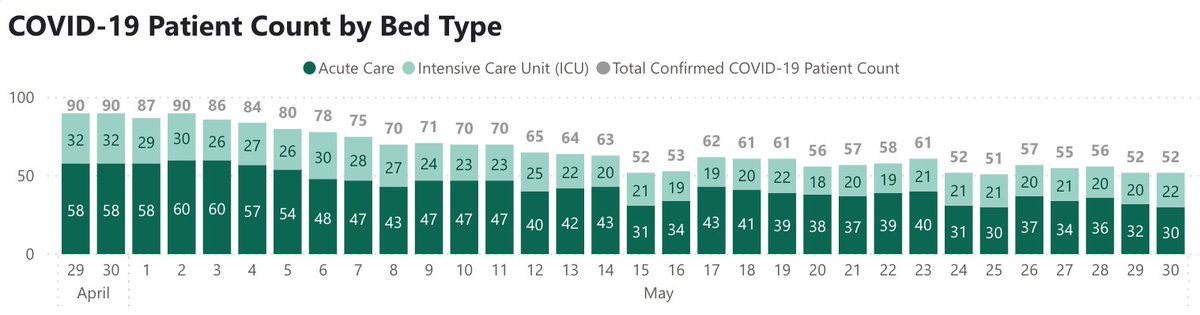
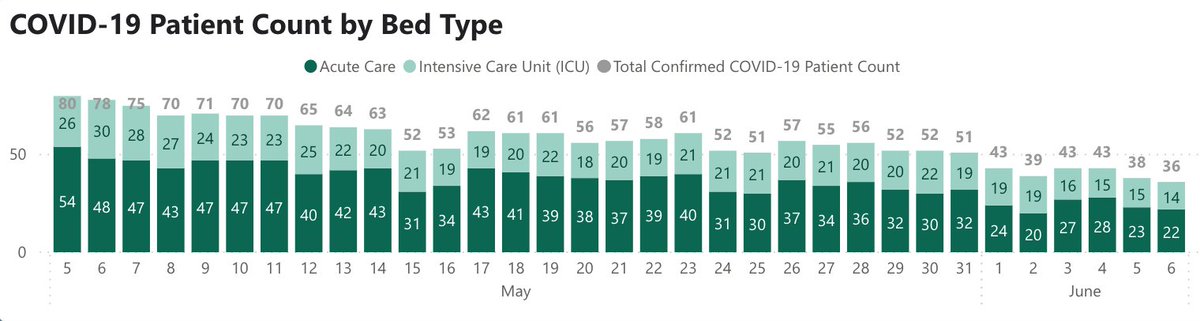
@ucsfhospitals, 10 pts, 2 on vents: fewest vented pts we’ve had since March.
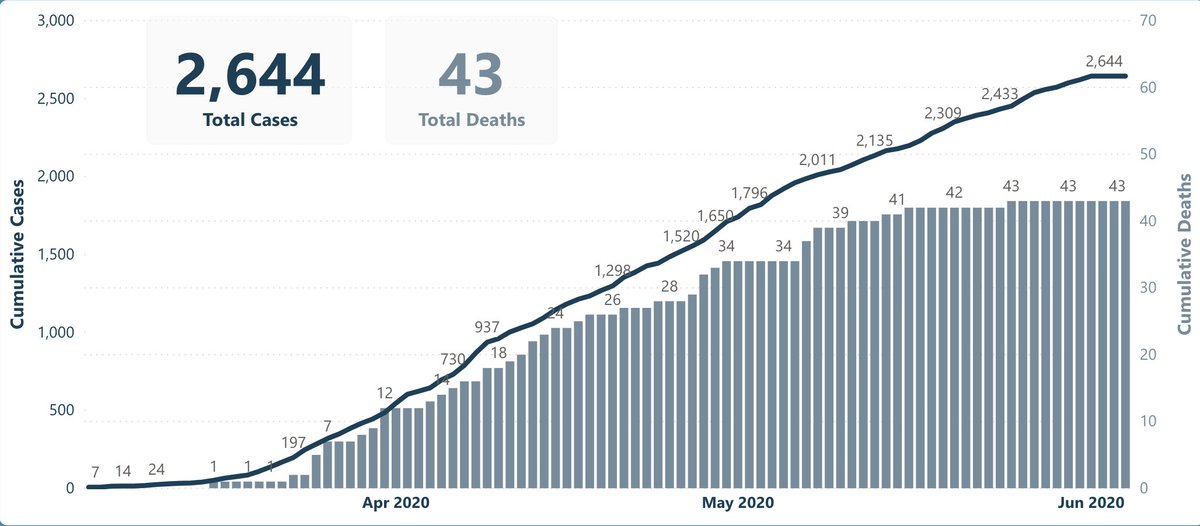
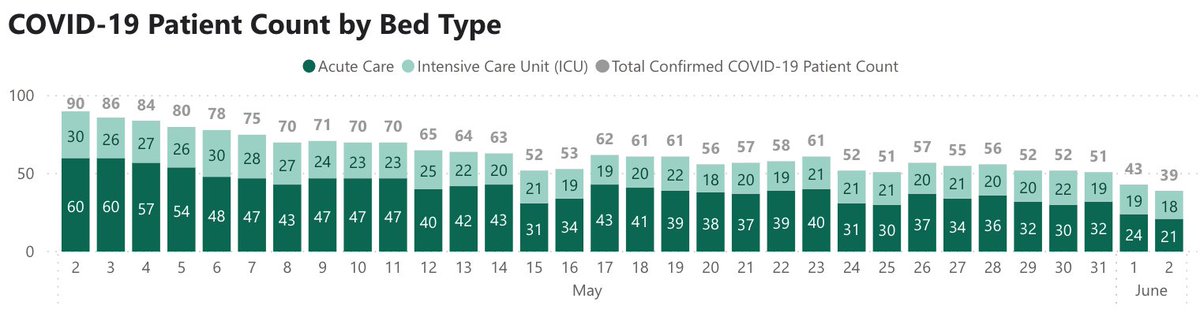
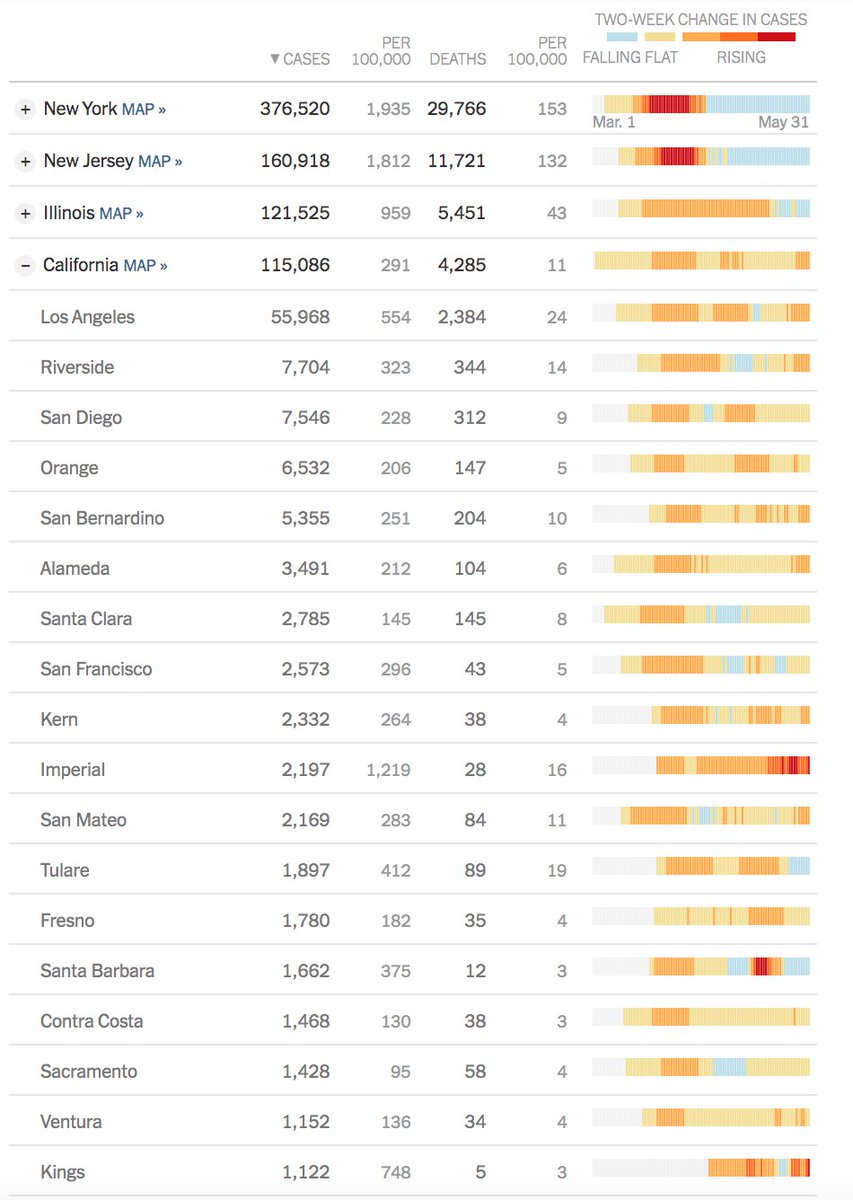
SF: new cases still ~25/d, but 0 deaths in 10 days. Hospitalizations down: 36, w/ 14 on vents – both #'s also lowest since March (Fig). CA surge all in southern CA
Hospitals care for the very sick, sometimes perform miracles, are where most Americans die, and are where we spend ~30% of our healthcare $'s. Hospitals were vital in Covid, but pandemic has dealt a huge blow to their bottom lines
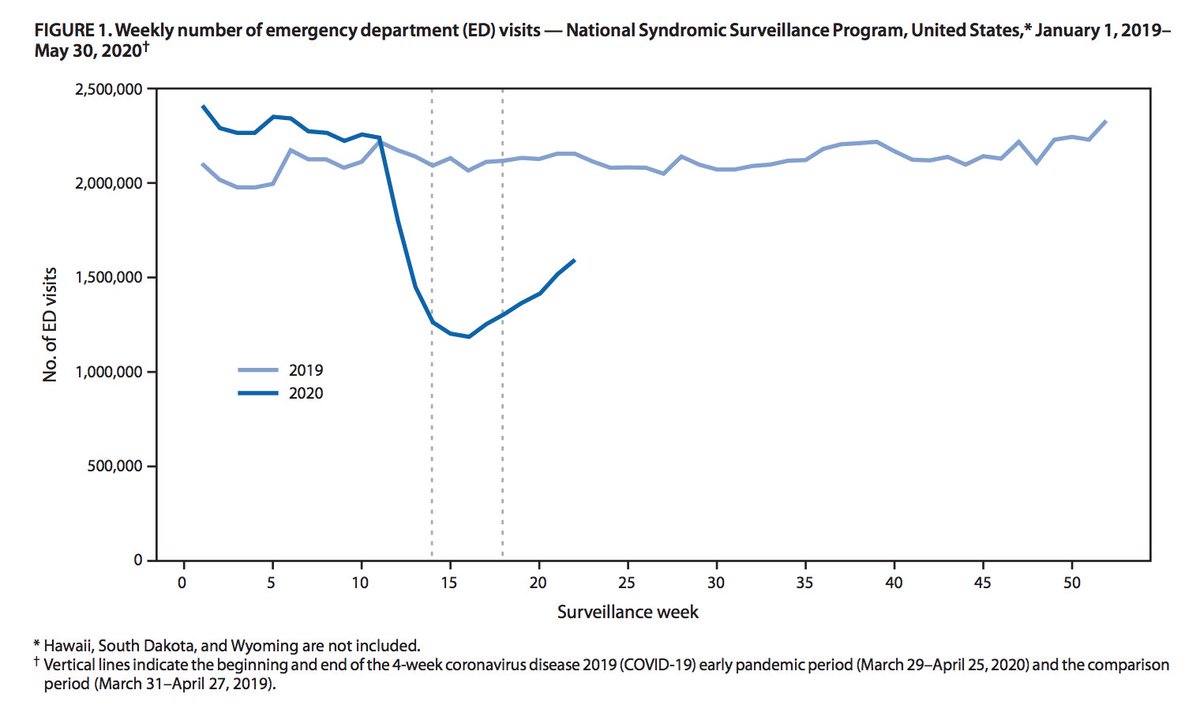
Re: telemedicine – we learned that not only can many (perhaps most) outpt visits go virtual, but also many hospital visits. This helped us lower # of visits (w/ lower PPE use & infection risk) & has big future implications.
Back Thurs for grand rounds. Stay safe.