
Chair, UCSF Dept of Medicine. Career: What happens when a poli sci major becomes an academic MD. Author, "A Giant Leap" on Health AI. Hubby/Dad/Grandpa/Golfer.
206 subscribers
How to get URL link on X (Twitter) App


 How am I acting currently? Given a moderate uptick in Covid over the past two months, I’m back to masking in crowded and poorly ventilated places, particularly when I don’t need to talk. When I do mask, I always use an N95; I see no reason to wear a less effective mask. (2/25)
How am I acting currently? Given a moderate uptick in Covid over the past two months, I’m back to masking in crowded and poorly ventilated places, particularly when I don’t need to talk. When I do mask, I always use an N95; I see no reason to wear a less effective mask. (2/25)




https://twitter.com/Bob_Wachter/status/1607162086282645505

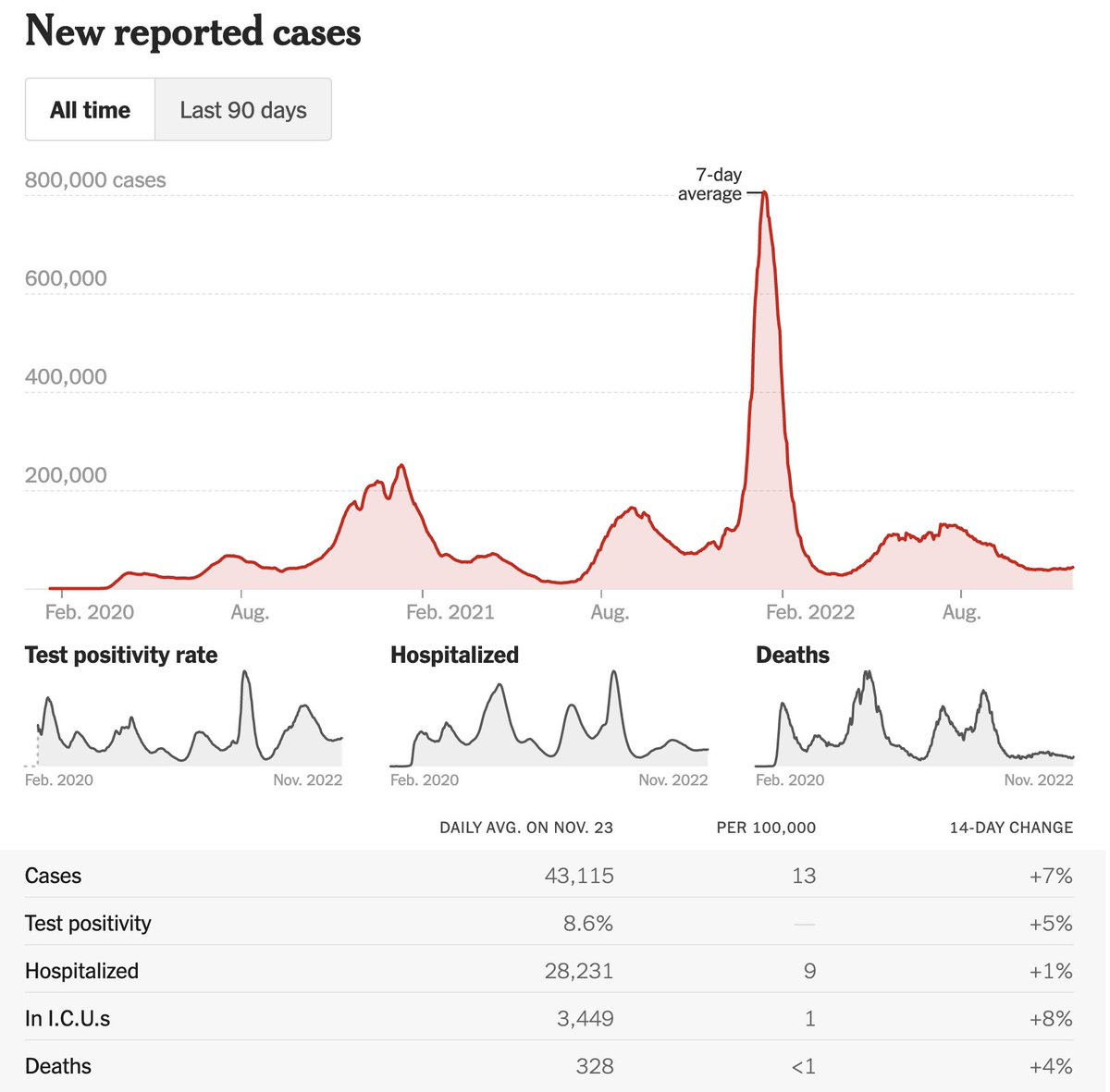



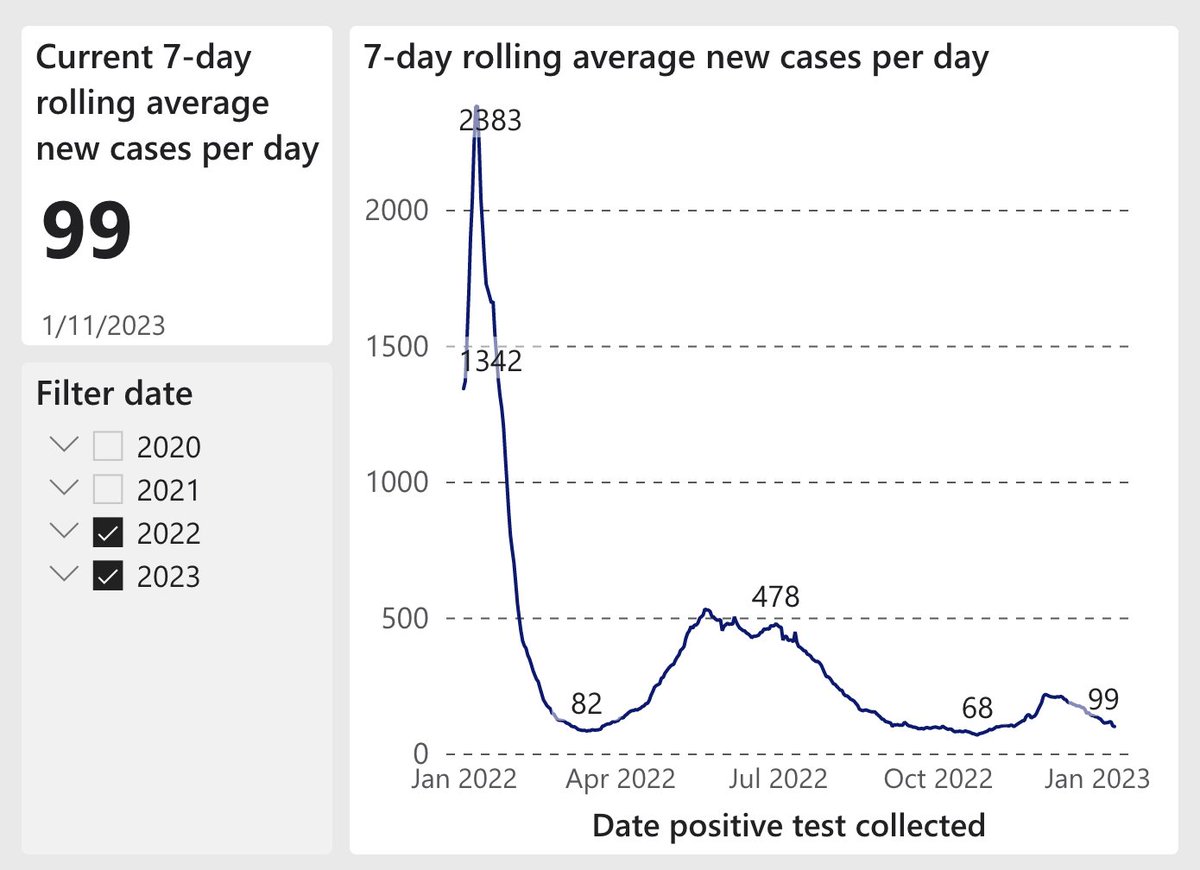
https://mobile.twitter.com/Bob_Wachter/status/1558234980706164736, cases in the U.S. have dropped steadily. Up until now, I’ve avoided indoor dining and worn a mask in all crowded indoor spaces. I’m now ready to eat indoors & (selectively) remove the mask. Here’s why: (1/25) As I said recently, my threshold to liberalize my behavior is <5 cases/100K/d in my region. (After accounting for home tests, 5/100K/d is really ~25/100K/d.) U.S. is now at 19, CA is at 12, & SF is at 6 (& fell 64% in past 2 wks). Find your # here:




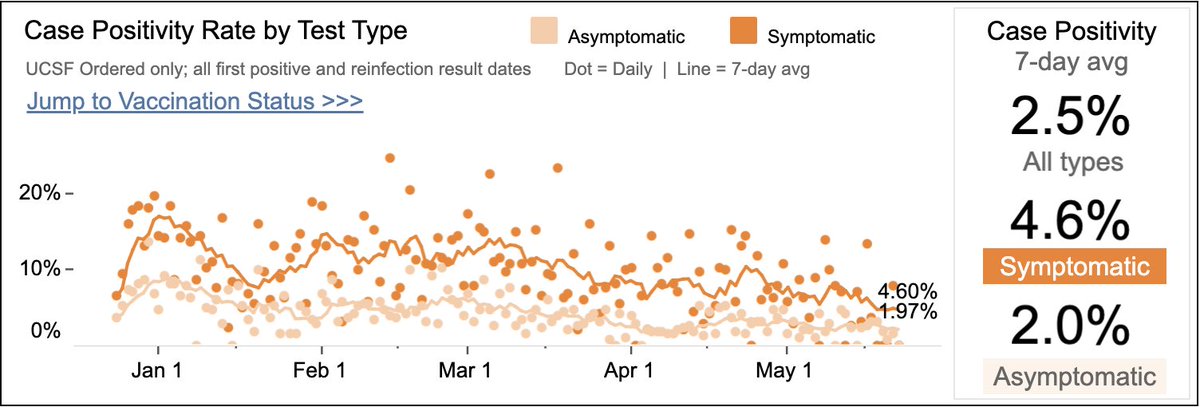
 @UCSFHospitals: 36 pts (6 ICU; ~50/50 “for” vs “with" Covid – Fig L). ⬇~30% in 2 mths; ⬇80% from Jan peak. Asymptomatic test pos. rate=3.6% (R); was ~6% 2 mths ago.
@UCSFHospitals: 36 pts (6 ICU; ~50/50 “for” vs “with" Covid – Fig L). ⬇~30% in 2 mths; ⬇80% from Jan peak. Asymptomatic test pos. rate=3.6% (R); was ~6% 2 mths ago. 





https://twitter.com/Bob_Wachter/status/1527026347117146112
