#Cardiotwitter @fpmorcerf Thread. The end ejection is also a complex series of events, with interaction between the aortic and mitral valves that is reflected in the septal and ring motions.
1/ The determining AVC by Tissue Doppler has been subject to confusion. In the septum, just after the ejection, there is a short negative spike. This was assumed to be IVR, among other things based on the proximity to peak negative dP/dt, which, however only is a proxy for AVC. 

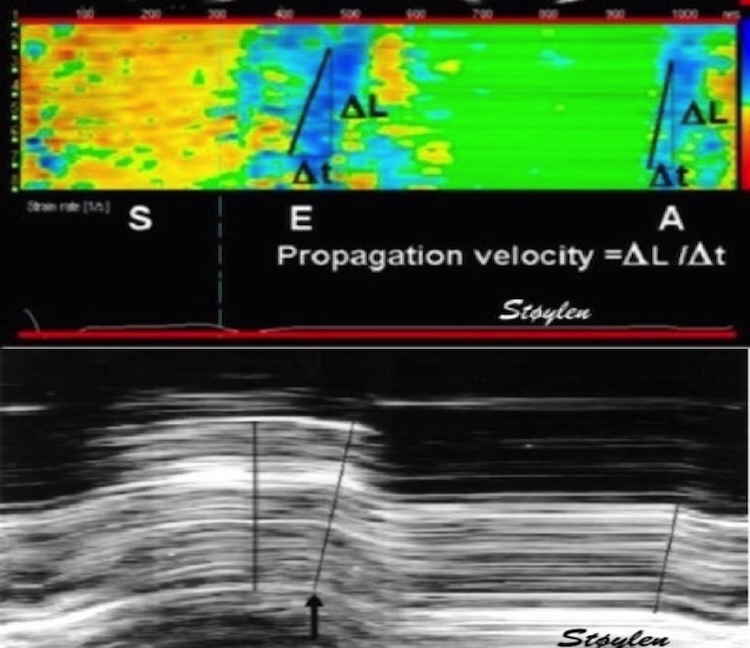
2/ This negative velocity is seen in both septal M-mode, spectral Tissue Doppler, colour TDI, and even as a septal elongation in strain rate. It was visual even in colour TDI of the mitral valve. Thus, AVC was assumed to be at the start of this event. 

3/ we have shown, both by phonocardiography pubmed.ncbi.nlm.nih.gov/16364793/ , by high frame rate B-mode of the aortic valve pubmed.ncbi.nlm.nih.gov/20331696/ that AVC occurred after this initial negative velocity. 

4/ and it is easily seen by transferring valve motions from Doppler flow to Tissue Doppler recordings, where it seems that this negative velocity is mainly septal. 

5/ so just as in the pre ejection spike, this is not IVR, and the true IVR (AVC to MVO) is from the end of the spike to start of mitral flow. 

6/ But is this interesting? Yes, firstly for correct measuring of IVRT by using TDI. Secondly, because this in itself gives information about aortic valve closure. Myocyte relaxation, in the meaning of tensjon development, starts at peak LV systolic pressure. 

7/ Shortening, continues, under decreasing tension, due to continuing, but decreasing outflow. At end of flow, there is no shortening, but continuing relaxation. This implies elongation with open aortic valve.
8/ The motion of the aortic root in a stationary blood column will in itself be a mechanism for closing the valve, and the valve closure itself be a mechanism for termination of this protodiastolic motion, but also the aortic orifice will "capture) a small volume at end ejection 

9/ This has been shown experimentally, pubmed.ncbi.nlm.nih.gov/18606917/, both the volume increase before AVC, and that stenting of the aortic valve abolished the protodiastolic spike. 

10/The protodiastolic motion of the mitral ring may be asymmetric, as the open aortic orifice will offer less resistance to the basal motion than the closed mitral valve 

unroll
@threadreaderapp
@threadreaderapp
• • •
Missing some Tweet in this thread? You can try to
force a refresh