⚡️What could cause ⬇️Na & ⬆️K in a neonate 👶?
🔥Let’s talk electrolytes with a paediatric 💫 in my first #Tweetorial @NSMCInternship @MedTweetorials
⚡️The Case⚡️
A 2⃣0⃣ day old male 👶 with lethargy &⬇️feeding
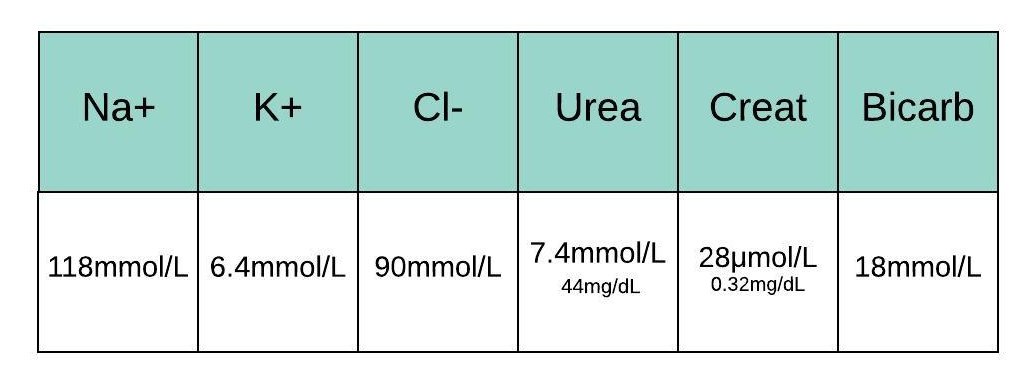
Bloods reveal hyponatremia & hyperkalemia
All of the above would be useful
1️⃣ Glucose is normal
2️⃣ VBG shows Metabolic Acidosis
3️⃣ Urinary 🧂 Sodium⬆️ & 🍌 Potassium⬇️
Remember
⚡️ The Anion Gap = Na+ - (Cl- +HCO3) ( =10 =Normal )
⚡️ Urinary Electrolytes should be measured before fluid resuscitation
⏰Time to start thinking about differential diagnoses⏰
What’s on your list for a sick infant with ⬇️ Na+ ⬆️K+ and NAGMA?
Let’s review 🔥Aldosterone🔥 to understand the biochemistry
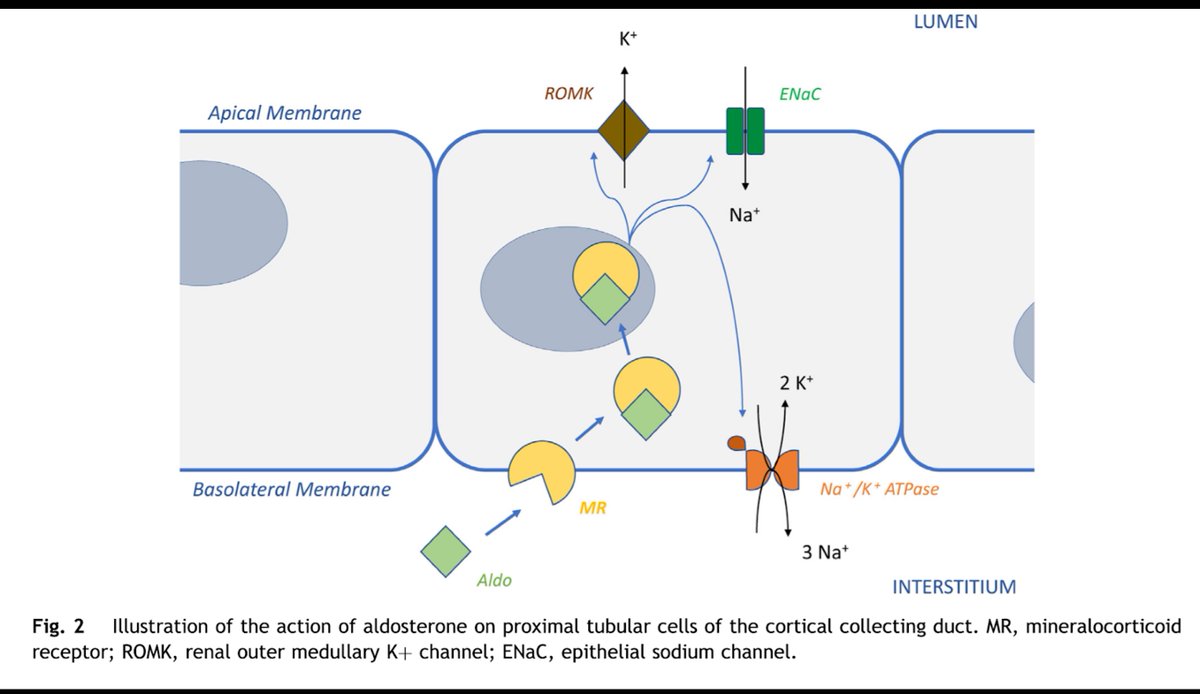
Aldosterone acts at the collecting duct via the MR on the principal cell to:
🅰️ ⬆️Na-K-ATPase pumps
🅱️ ⬆️ENaC expression
↪️ Na in & K out (via electrical gradient created)
pubmed.ncbi.nlm.nih.gov/30962012/
In summary:
Aldosterone ➡️➡️
1⃣Na+ reabsorption
2⃣K+ and H+ excretion
⚡️ Therefore - our baby’s presentation with ⬇️ Na+ ⬆️K+ and #NAGMA fits with ⬇️ Aldosterone⚡️
⚡️This presentation is described as a Type 4 Renal Tubular Acidosis ⚡️
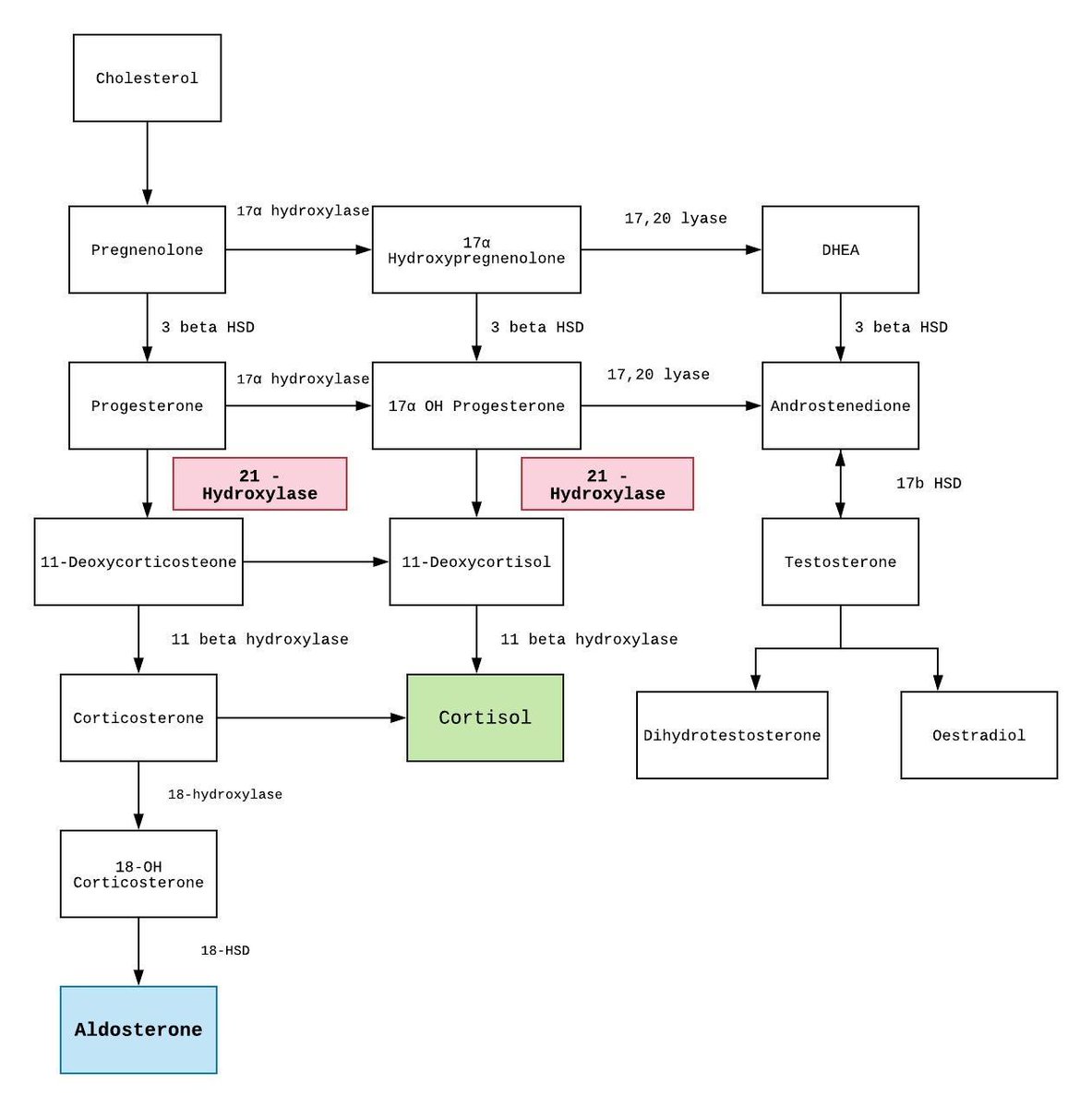
Given what we have reviewed about aldosterone➡️
hypoaldosteronism secondary to 21-OH CAH is a valid differential. But it is not the only possibility.
What other investigations might you consider at this point?
All of the above are appropriate.
Our baby has ⬆️leukocytes and organisms 🐛 in his urine.
Renal US shows bilateral hydronephrosis
Cortisol is appropriate and 17OHP is Normal
Plasma renin & aldosterone are markedly elevated ⬆️⬆️
🔥Infants with UTI can develop transient tubular resistance to aldosterone🔥
This form of pseudohypoaldosteronism (PHA) can mimic the biochemical picture seen in CAH
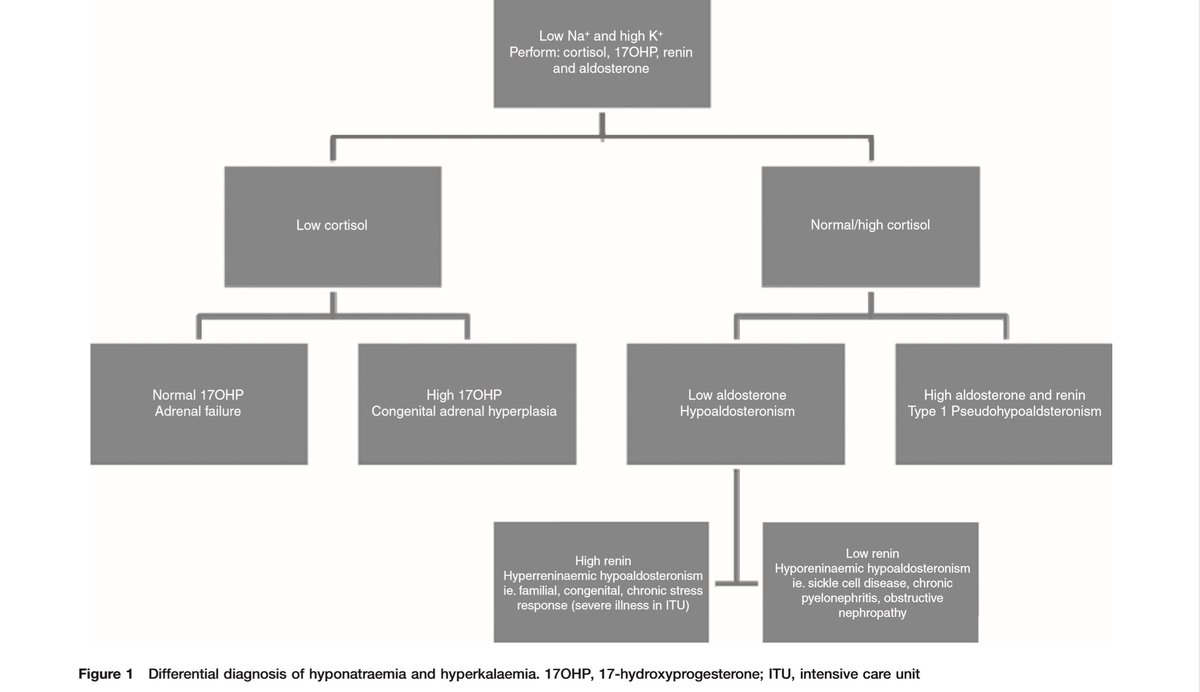
An approach to distinguishing them ⬇️
⚡️Glucose can also be helpful⚡️
pubmed.ncbi.nlm.nih.gov/21525149/
Transient PHA is also known as Secondary Type 1 PHA.
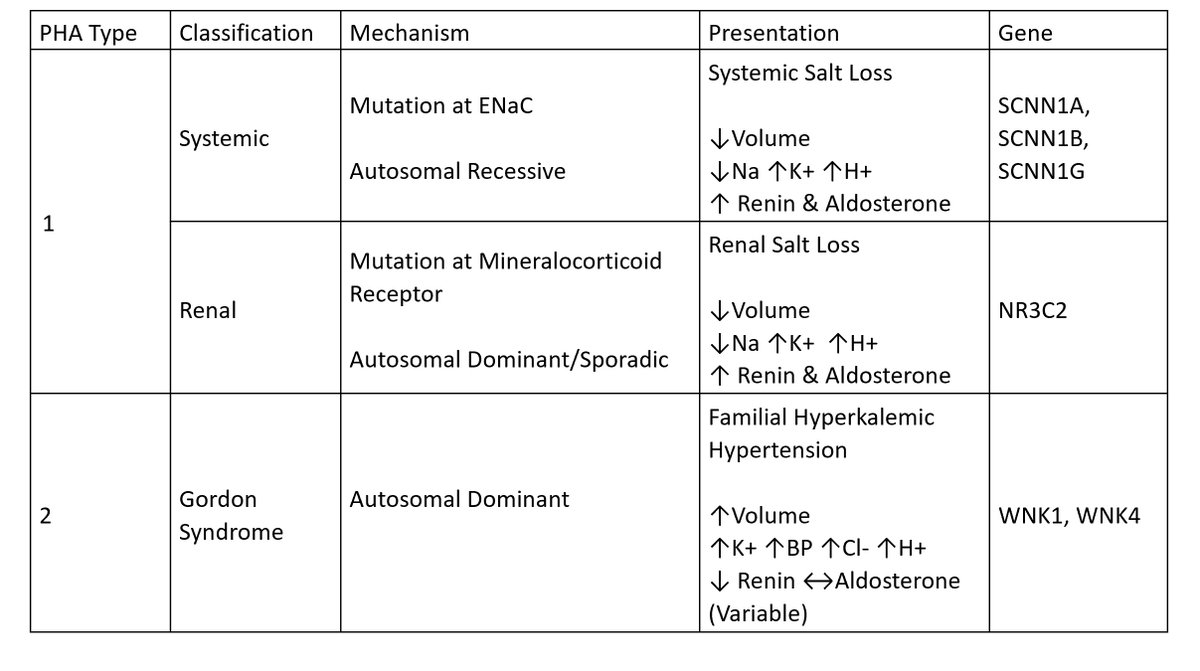
Primary (genetic) forms of PHA also exist which are unrelated to UTI. These are summarised below⬇️
A more detailed review is provided at pubmed.ncbi.nlm.nih.gov/23392097/
The pathophysiology of transient/secondary PHA is unclear
⬆️ intrarenal pressures ➕ inflammation➡️parenchymal damage ➡️ tubular unresponsiveness to aldosterone is proposed
⚡️Tubular immaturity in infants 👶 may also play a role⚡️
(PMID: 30962012) (PMID: 25043099)
Some facts about transient PHA
⚡️Can be induced by UTI & urinary tract malformation - together or separately (PMID 30962012)
⚡️Electrolyte disturbances resolve with fluid mgmt & UTI treatment
⚡️Most cases are in infants< 6 months, BUT can be older (PMID: 30962012)
Transient PHA is rare and under-recognised
⚡The annual incidence of transient PHA was similar to “salt losing” CAH in an Irish Review (adc.bmj.com/content/104/Su…)
⚡Always consider transient PHA when you see this electrolyte pattern (⬇️🧂⬆️🍌) in an infant⚡