Starting now! Follow along with #DPACOVIDSeries 
Kima Taylor kicking off the panel by highlighting the fact that treatment will not 'fix' all our problems and we have to think about substance use more broadly and the holistic needs and systems needed to address people's needs.
And that we cannot look at substance use without zooming out and thinking about the racialized war on drugs that started out as a war on communities of color, particularly around the labor threat they posed to white Americans.
So with that consideration, we should examine how we talk about drugs, incarceration, treatment access, and race.
Now highlighting the opioid crisis and that it did 2 things: 1) it gave addiction a white face and started conversations about pain and meds, and 2) it placed the blame of addiction on the 'other' - doctors. Taylor acknowledges her role as a provider in this part.
This created a false dichotomy that went along racialized lines (bc whites started with pills, but unmedicated Black communities were always using street drugs), but also pushed conversations about harm reduction to the margins. Absorbing some interventions differently.
And then to think about what this meant for MAT - we need to acknowledge how race, class and social control always dictated methadone dispensing and impacted how bupe was differently marketed for suburban whites. COVID only made this clearer. Bupe still EASIER to access now too.
Taylor wrapped by talking about how current uprisings also highlight the need for nuance when making asks for reinvestment and not limiting imagination to continuum of care of HR to MAT; but also to put housing, social services, and other services on that continuum.
Now @losanjalis talking about her Casa de Salud work- they are not an FQHC, they are a non-profit that aims to provide holistic services - mind/body/soul - in a culturally- and community-sensitive manner.
.@losanjalis speaking about how NM has had generational trauma, racism, criminalization, and opioid use - well before the current "opioid" crisis.
We say "come for the suboxone, and stay for whatever else you want to" @losanjalis - the organization starts where clients are at and encourages participants to use any combination of the myriad services they provide.
"Two out of every three narcan kits that were distributed in May were used to save a life" - all of this during #COVID19 @losanjalis. All of this while the community is facing employment and economic challenges and stressors around the crisis.
.@losanjalis speaking about the opportunity during #COVID19 in light of buprenoprhine initiation policy changes. We can ask ourselves - "What do we want to keep from this and how do we want to make that happen"
Now Roopa Sethi speaking about her work in Kansas at her methadone clinic. One challenge that emerged is that despite easier prescribing of buprenorphine, they saw that pharmacies did not have enough supply to fill scripts.
Another challenge involved self-pay clients who were no longer able to use certain coupons to offset some costs/expenses of filling buprenorphine prescriptions.
The use of telehealth technology like zoom or those that required smartphones was also a challenge so they ended up shifting all services to telephone sessions as a result. This is an important consideration when thinking about reimbursement.
Re: methadone dispensing, her clinic opted to allow 7 days of take-homes for 'less stable' patients and 2-3 weeks of take-homes for "more stable" patients. She said they have seen benefits in many patients who didn't need to attend so frequently.
Because of physical examinations that remained mandatory for methadone patients, it remained a challenge for providers and the staff.
Now we are hearing from Lisa Puglisi of Yale, speaking of her work in New Haven in CT and how experiences have changed in #COVID19. She is a PCP and takes a chronic care approach and looking at concerns in a holistic manner.
Puglisi is really thinking about MAT and surveillance - in ways that are similar to the surveillance of the criminal justice system. "You have to be 'good' to get started. And if you're good, your prize is you get an extra day of your life back" In #COVID19, this has gone down
And that it frees up patients from the observation of the community, of taking the bus, of having potentially degrading experiences with providers in the OTP, of the observed drug testing, etc.
Given the "infantalising" nature of treatment, people are now feeling free, explains Puglisi. She hears a "sign of relief" from her patients about not being subjected to these restrictions anymore.
Beyond reduced surveillance of OTP, clients are also telling her the sigh of relief of being less surveilled by probation or parole now as well. People are feeling free, able to focus on family, self-care, and other responsibilities.
Decreased surveillance has helped Puglisi as a provider because she can "actually practice medicine and build relationships" because surveillance systems of parole and probation can't "pluck" her patients out of care now either.
"I'll do anything to advocate - call POs, write letters- yet I'm ultimately not in control of the outcome there" Puglisi says that the decreased surveillance can really teach us about how care can be improved without these threats to care.
Puglisi saying that her preliminary research suggests that decarceration has led to dramatically positive health outcomes and that this must be accompanied by coordinated health and social services. You need a robust system that communicates with itself.
Puglisi talking about the improved communication now also possible due to #COVID19 wherein providers have greater access to information and can better collaborate to meet clients' needs. But she also notes- if it could happen this quickly, it should have always been like this!
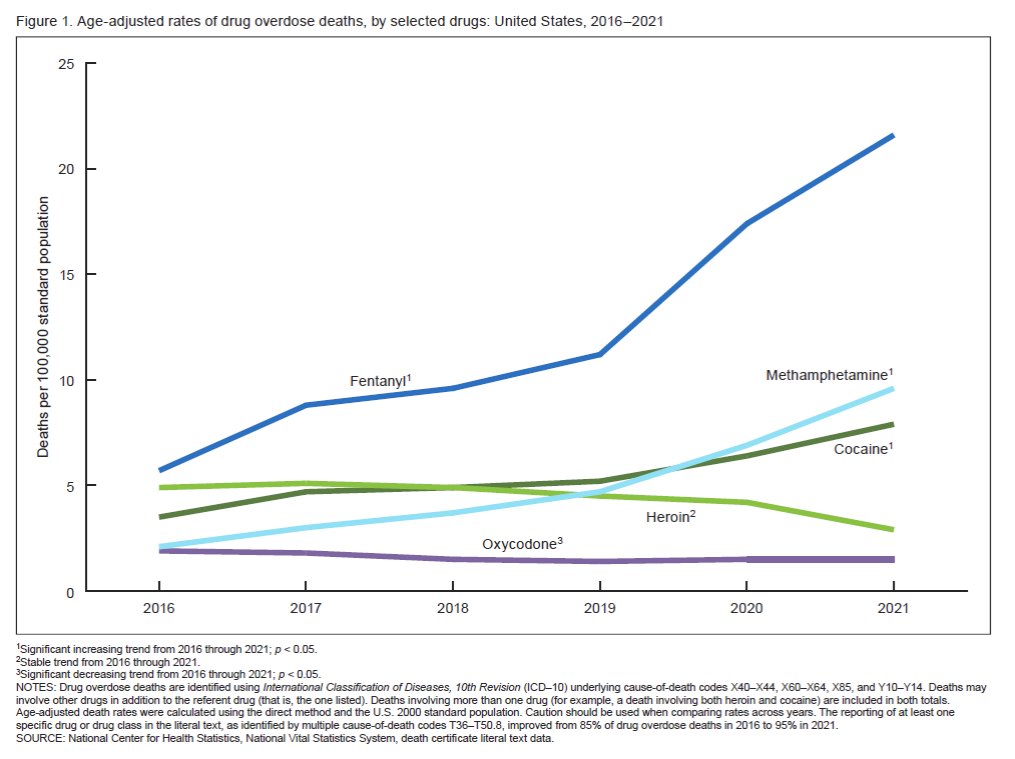
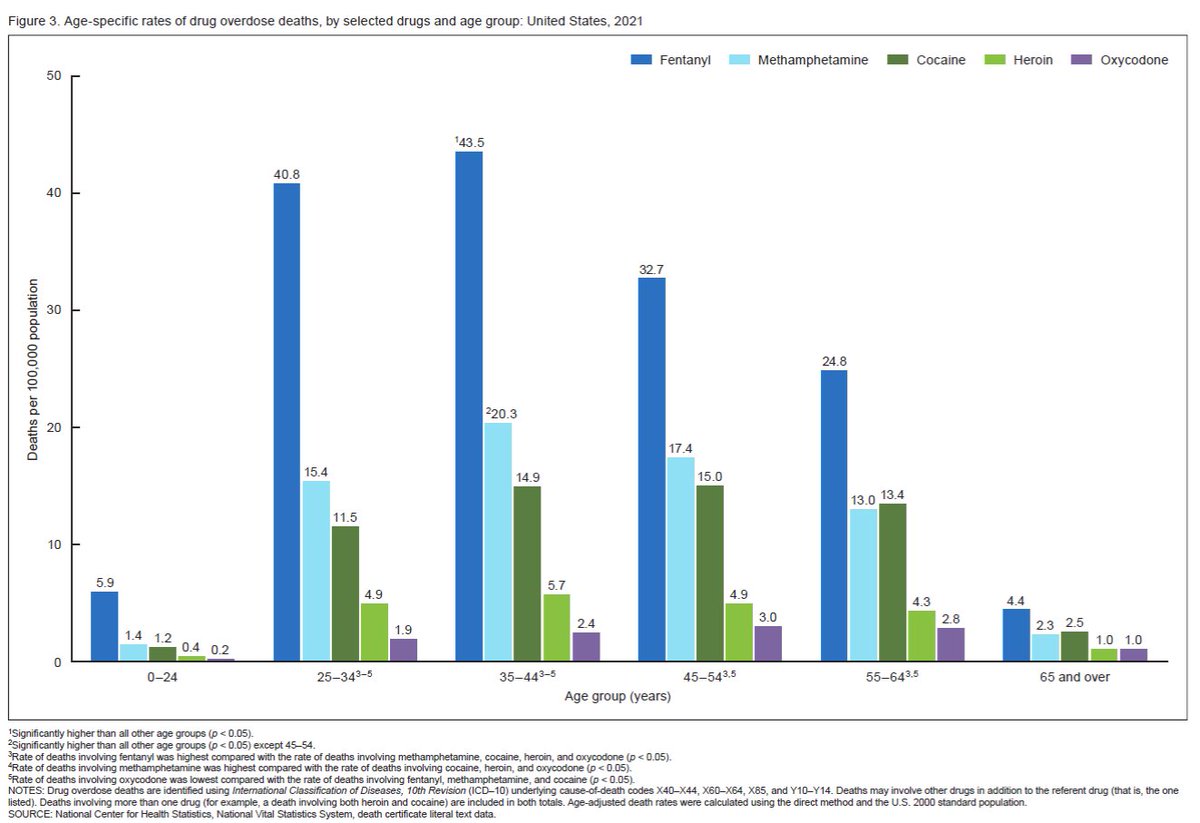
Now Richard Rawson invited to speak about the treatment needs and options for people who use stimulants. He notes - it's such a different conversation than what's happening with people who use opioids.
He's been working to try to bring flexibility as a "brand new concept" for people who treat those who use stimulants, since treatment was historically abstinence-oriented.
He is talking about 3 populations: 1) ppl seeking specialty care for stimulant use disorders; 2) ppl with opioid use disorders who also use stimulants; and 3) people who use stimulants harmfully who aren't seeking care. He will talk mostly about people in 1.
He is discussing how contingency management, a treatment grounded in behavioral theory that uses incentives to promote behavior change. It has best evidence for stimulant use disorders, but insurance reimbursement and staff attitudes remain barriers.
He is sharing ReSet and Dynamic Care, two apps that have potential for being used for CM for stimulant use disorders.
He is working hard with providers to change their attitudes to enhance retention, offer a menu of options (incl exercise to help with w/d, craving, depression, etc.), and to find a way to integrate elements of CM into their work. Retention/engagement should be goals.
Rawson highlighting that methamphetamine hysteria is detracting from being able to focus on cocaine as well- you can't just think of white rural methamphetamine users without thinking of urban Black cocaine users too. Have to acknowledge race/class/geog elements.
Some barriers to CM implementation include: staff attitudes, getting money for CM rewards, and insurance such as Medicaid won't allow these cash reimbursement.
We @DrugPolicyOrg hosted a conference on Stimulant use, treament and harm reduction in 2017. You can see the program and summary report (I wrote it!) here: drugpolicy.org/event/stimulan…
@DrugPolicyOrg Who is left out now? Panelists now discussing those with low technology, pregnant people, lacking infrastructure, homeless, etc. And we still need better data to identify whose needs are/are not met. Puglisi talking about the need to also look at more outcomes/benefits.
We should challenge looking at urine drug tests as a metric of success - what about looking at quality of life, civic engagement, relationships, etc - as success of treatment and benefits of reduced structure for treatment during COVID19
So how do we talking about reinvestment now in a way that's helpful? Taylor now saying we should be thoughtful about what we're asking and make sure to include patient-centered services along with accountability/outcome measures that make sense for health/wellbeing.
Puglisi giving @DrAyanaJordan's Imani program a shout-out right now- highlighting that evidence-informed programs that are administered by trained and trusted community members can be effective, tailored, and don't need to be costly- contrary to popular belief!
But amazing programs like this are fighting for funding and should be considered for reinvestment funding since insurance will not cover it. We need to think about how to pay them adequately and allow them to function and sustain themselves. This means peer work too! -Taylor
What should research look like in light of #COVID19? Puglisi speaking to the need for client-driven research. For more info on this, check out @DrugPolicyNerds resources for democratizing research: drugpolicy.org/event/ethics-e…
You can also join @DrugPolicyNerds Google Group about conducting research on drug use, overdose, harm reduction, treatment, etc. in light of #COVID19 - drugpolicy.org/resource/rapid… email me at svakharia [at] drugpolicy [dot] org
**Sorry but my internet keeps cutting out during Q & A**
• • •
Missing some Tweet in this thread? You can try to
force a refresh