Part 1 of 2
19M +3 wks fever, confusion. Exam notable👇. Brain MRI +frontal lobe masses. CSF: lymph pleo, low gluc. CSF/blood cx, viral PCRs, Histo/Crypto/Blasto/Cocci(-). IGRA/AFB smear/Cx (-). Brain bx: granuloma, +necrosis, AFB/GMS/Cx(-). No response to Abx. 👉 Part 2
19M +3 wks fever, confusion. Exam notable👇. Brain MRI +frontal lobe masses. CSF: lymph pleo, low gluc. CSF/blood cx, viral PCRs, Histo/Crypto/Blasto/Cocci(-). IGRA/AFB smear/Cx (-). Brain bx: granuloma, +necrosis, AFB/GMS/Cx(-). No response to Abx. 👉 Part 2

Part 2 of 2
Previously healthy, no PMH exc for recent dx of “skin TB” when he p/w nasal skin lesion 👆that showed granuloma w/ (-)AFB/GMS on skin bx. Started on RIPE 2 mos prior to presentation. Lives in rural Minnesota, (-)travel. Given SSx, w/c of the ff is the most likely Dx?
Previously healthy, no PMH exc for recent dx of “skin TB” when he p/w nasal skin lesion 👆that showed granuloma w/ (-)AFB/GMS on skin bx. Started on RIPE 2 mos prior to presentation. Lives in rural Minnesota, (-)travel. Given SSx, w/c of the ff is the most likely Dx?
1/11 50% got the right answer! Nice job. A case of Balamuthia mandrillaris.
Balamuthia, one of the free-living ameba pathogenic to humans (like Naegleria & Acanthamoeba). Like Acanthamoeba, causes granulomatous amebic encepahlitis (GAE).
Pic in MCQ from bit.ly/2YNQFjs
Balamuthia, one of the free-living ameba pathogenic to humans (like Naegleria & Acanthamoeba). Like Acanthamoeba, causes granulomatous amebic encepahlitis (GAE).
Pic in MCQ from bit.ly/2YNQFjs
2/11 Balamuthia GAE causes brain abscesses, that maybe ring-enhancing & a/w edema/hemorrhage. Patients p/w headache, seizure, confusion, fever. CSF shows lymphocytic pleocytosis, high protein, and low-normal glucose 👉 difficult to distinguish from fungal/TB CNS infection.
3/11 As @RicardoLaHozMD pointed, one very helpful clue to Balamuthia is the presence of a characteristic rash in the central face/nose the usually precedes the onset of GAE by 2 wks to 2 yrs and is almost always visible on exam.
4/11 Note that this characteristic rash is almost always present in cases reported outside of the US (e.g. Peru) bit.ly/2YEDt09. But this is uncommonly reported in the US (only 6% of cases) bit.ly/2CfP4ev .
5/11 Nevertheless, in a patient who p/w brain abscesses, skin exam could give you clues and can lead to early diagnosis (think Nocardia). Rash, usually painless, nodular-plaque in the central face but can also be in the extremities 👇bit.ly/2Y5Quk9 (esp elbow/knees). 

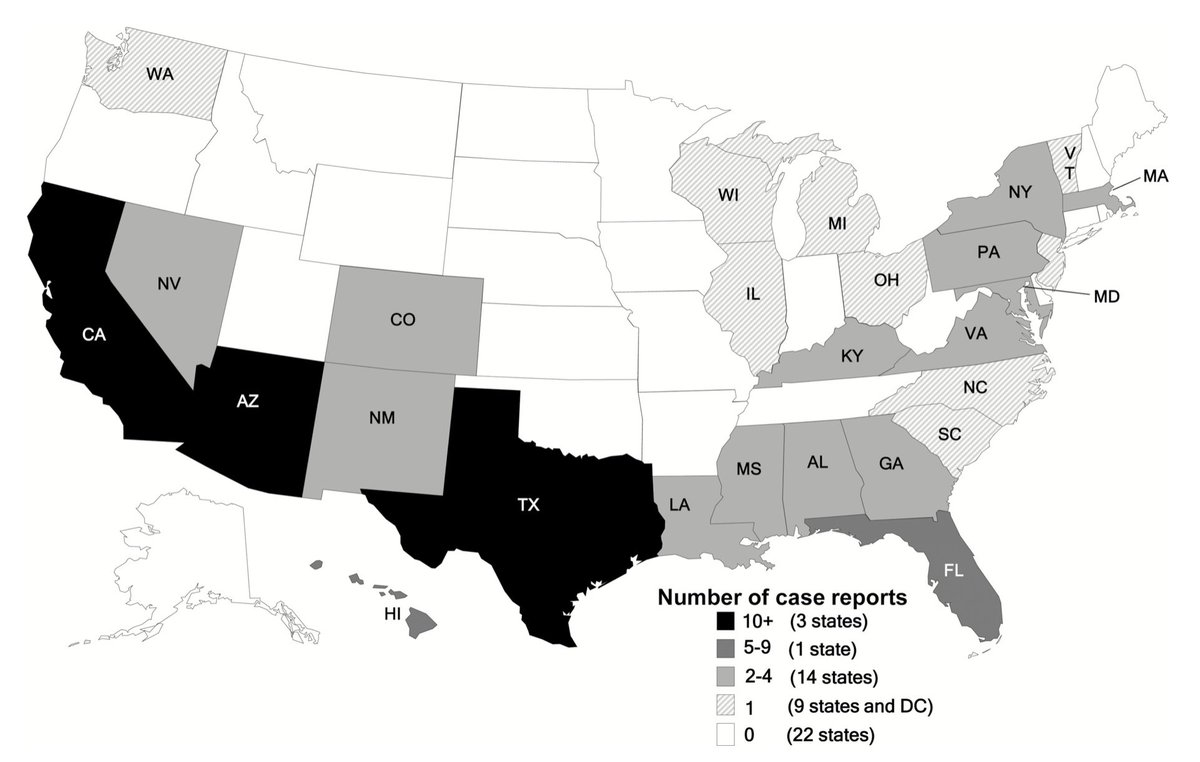
6/11 Balamuthia, reported worldwide. US, common in California, Arizona and Texas👇bit.ly/2CfP4ev. The ecological niche of Balamuthia is not well defined, unlike Naegleria & Acanthamoeba (water). Patients usually report soil > water exposure ‼️ bit.ly/30Ojvmf 
7/11 Diagnosis is challenging 👉 usually requires brain biopsy. Unlike Naegleria, ameba is not usually seen in CSF. H&E and PAS staining of tissues to see trophozoites & cysts. Requires PCR testing of tissues in most cases (hard to distinguish from Acanthamoeba on microscopy).
8/11 Balamuthia is a fatal disease. Treatment is usually delayed (esp in cases w/ no skin lesion) and ineffective (combination of different antimicrobials including: pentamidine, sulfadiazine, flucytosine, miltefosine).
9/11 Refer to Table 👇 that summarizes the key features of Balamuthia GAE as compared to Acanthamoeba & Naegleria. #highyield @grepmeded 

10/11 In summary, include Balamuthia in your DDX for brain abscesses of unknown etiology, esp in those w/ concurrent/preceding nasal/central face skin lesion. Closest DDX: fungal and TB. May require brain biopsy, contact health department to help w/ testing.
One more thing...
One more thing...
11/11 I always think that midline face/nose lesions can sometimes help you generalte DDX. See Table 👇 @grepmeded #highyield . A case of Klebsiella rhinoscleromatis was one of the first cases we featured here at @WuidQ 2 years ago 👉 
https://twitter.com/wuidq/status/1025353508705501184?s=21

• • •
Missing some Tweet in this thread? You can try to
force a refresh