Great work!
Many have been calling it practice changing and have suggested Dexa should be used in all patients admitted and in need of oxygen or mechanical ventilation.
I am way less comfortable with the interpretation.
Short summary:
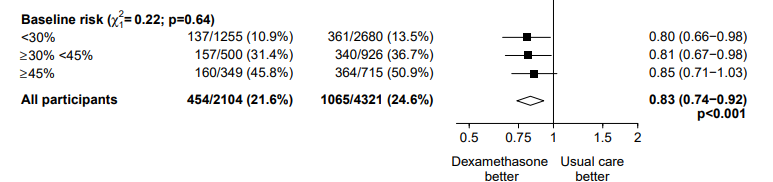
Dexa vs. usual care = 3% absolute risk reduction /14% relative risk reduction.
Subgroup analysis by respiratory support showing effect modification.
Those on oxygen and those on a vent had benefit (aHR 0.80 and 0.65).
The conclusion suggests anyone on oxygen or on a ventilator would benefit and should be treated w/ Dexa
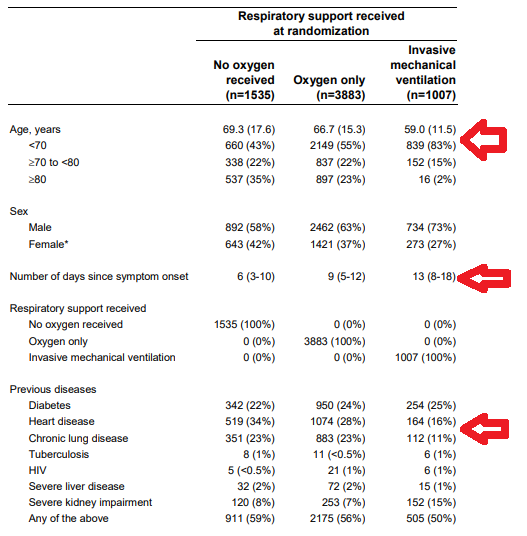
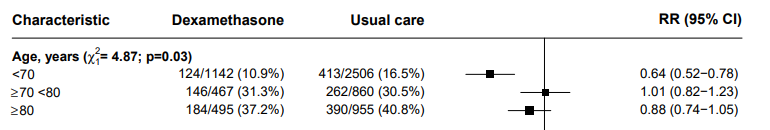
Although the study is balanced across treatments it is not balanced across subgroups.
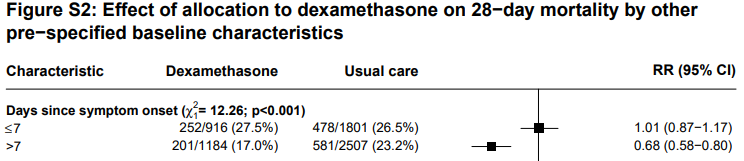
If yes, can this be the real factor leading to differences in benefit by treatment?
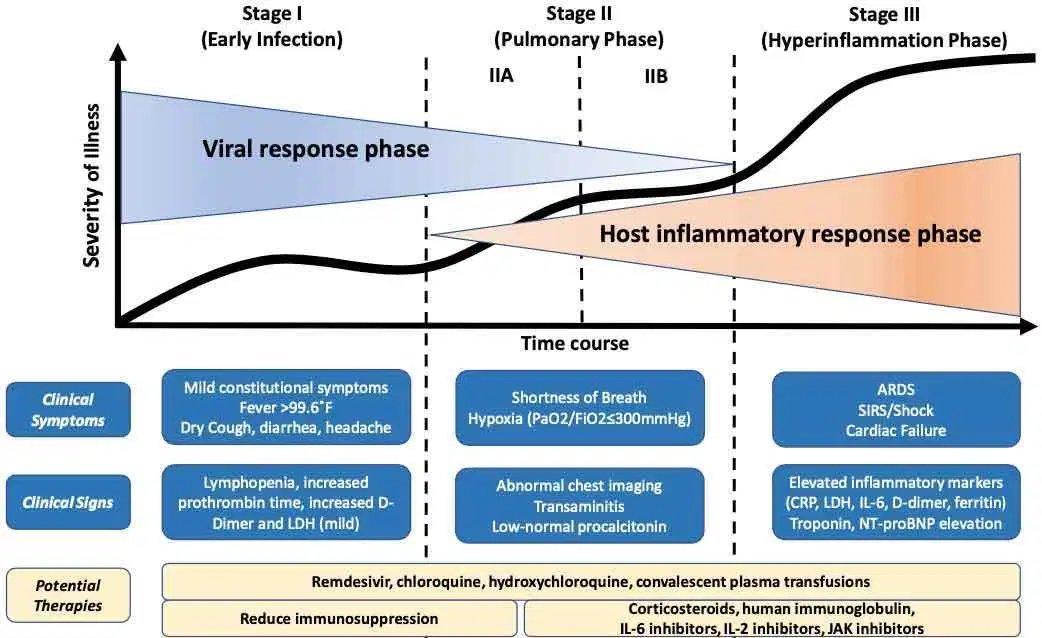
Is there a rationale for this?
I would say yes twice for all of those questions
So, interpretation 1: The effect of dexa could likely be dependent on time (better late) rather than ventilatory support.
The more severe group is 10y younger (69 vs. 59) and has lower prevalence of heart (16% vs. 34%) and lung disease (11% vs. 34%).
This means the more severe group is less frail. Can this be the effect modifier?
A. more frail, older individuals are less likely to develop immune over response, thus less likely to benefit from immunomodulation.
B. Those individuals also more likely to develop secondary infections, critical care neuropathy, etc.
I´ll end with a question based on the study and my comments. Who do you think is probably the key factor to decide when to use Dexa based on RECOVERY?