Grand rounds today: . As we hit Covid’s 6 month mark in the U.S., we’re desperate for innovative approaches. Today, I decided to focus on 3 impressive ones – across a range of disciplines: testing, epi, & narrative.
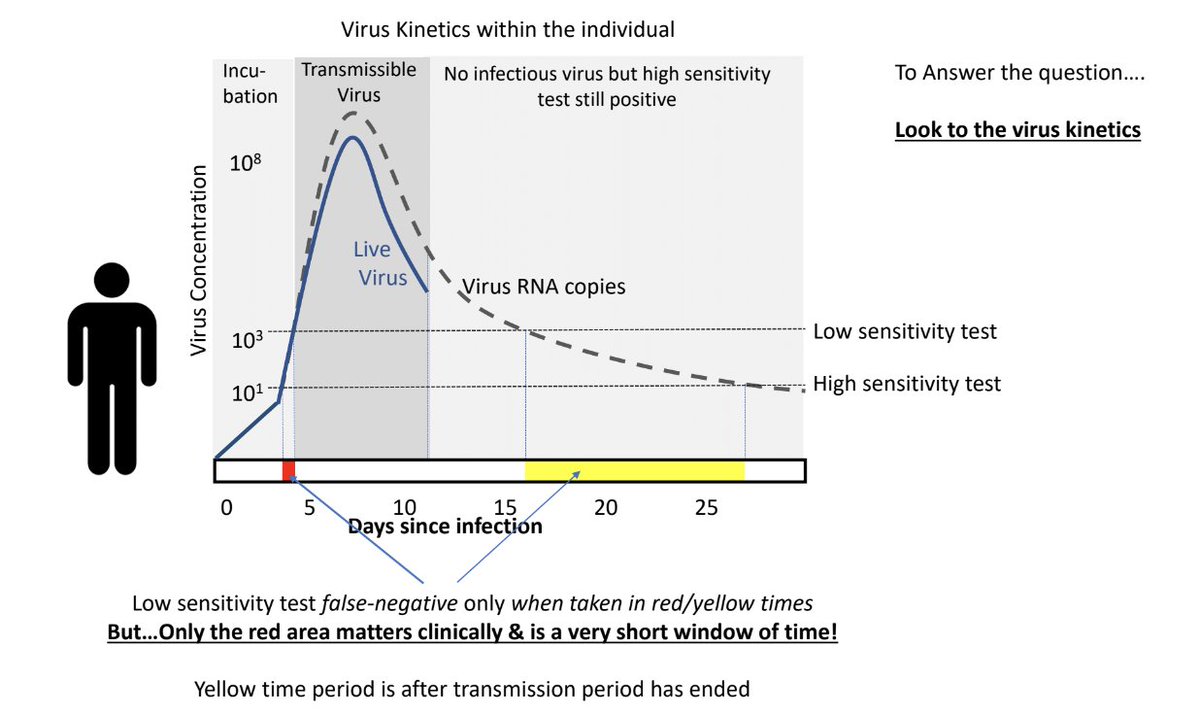
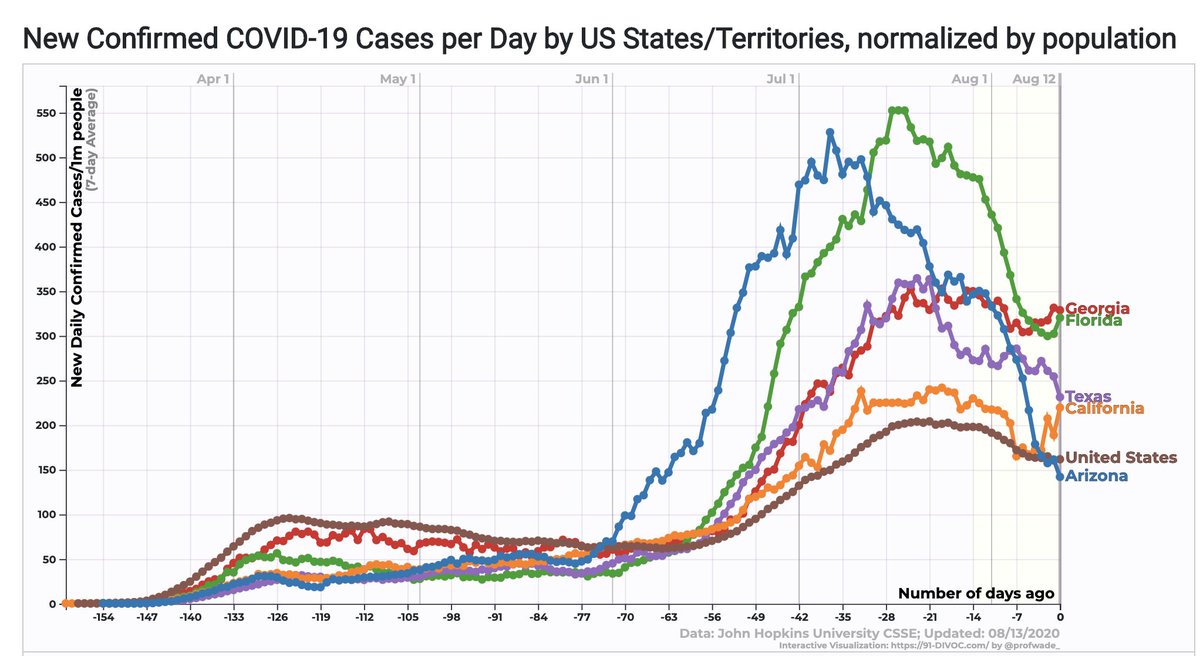
But he feels that his job is to describe science clearly. Which he did.