The SGLT2 inhibitors are now officially not ‘diabetes’ medications, but also drugs capable of risk reduction for people with heart failure and reduced systolic function. And more than one option. All good news for patients. Now to ensure access. #ESCCongress #ESC2020 @TheLancet 
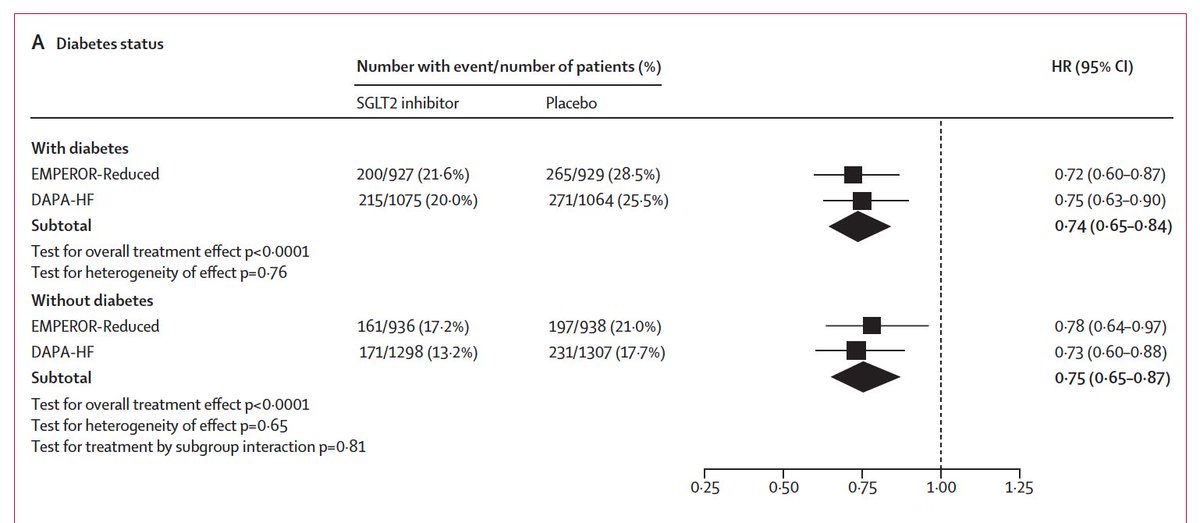
@TheLancet The key thing about the meta-analysis of the SGLT2 inhibitors is that the primary endpoint was The primary endpoint was time to all-cause death. Not a composite. Not something needing adjudication. 13% reduction in allcause death (pooled HR 0·87, 95% CI 0·77–0·98; p=0·018).
@TheLancet The absolute difference in deaths was 1-2% range; but when you look across other outcomes, including hospitalizations, it is substantial. For adverse effects, interestingly, severe hypoglycaemic events was low, with
no increase in the active treatment groups in both trials.
no increase in the active treatment groups in both trials.
Reproducibility means a lot to me. Too often we are not testing reproducibility-or class effects. The authors note: 'striking consistency of the findings of CV and renal benefits w/empagliflozin & dapagliflozin in patients with HFrEF
across the two trials.’ #ESCCongress #ESC2020
across the two trials.’ #ESCCongress #ESC2020
• • •
Missing some Tweet in this thread? You can try to
force a refresh