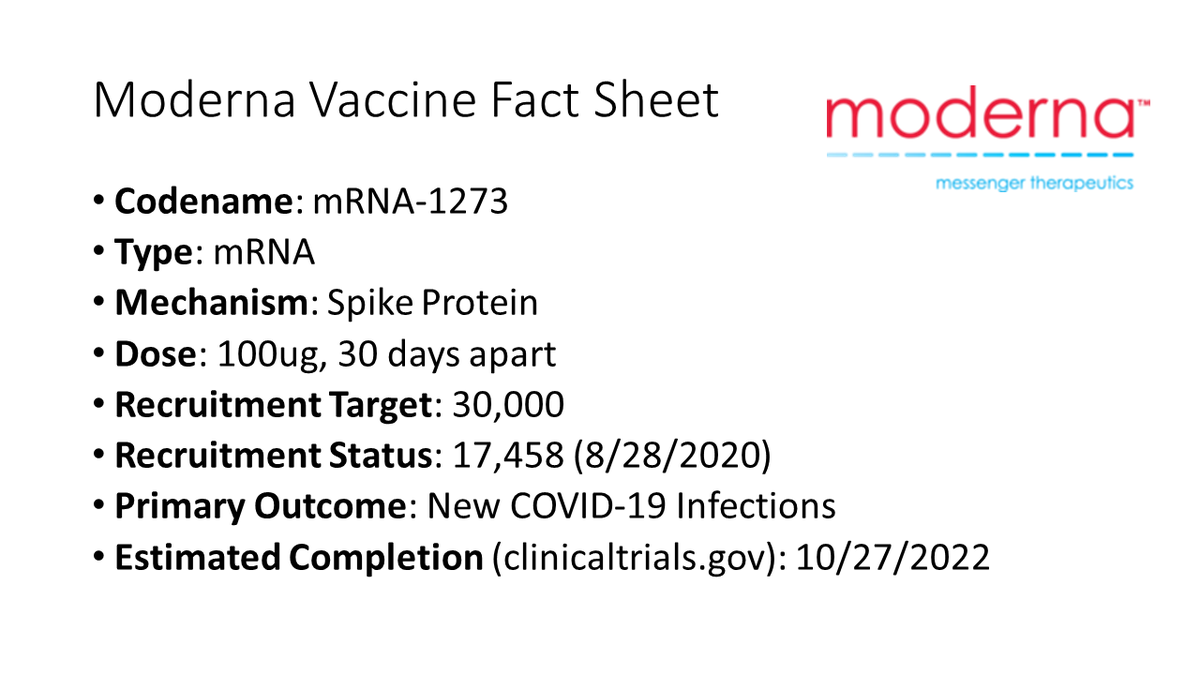
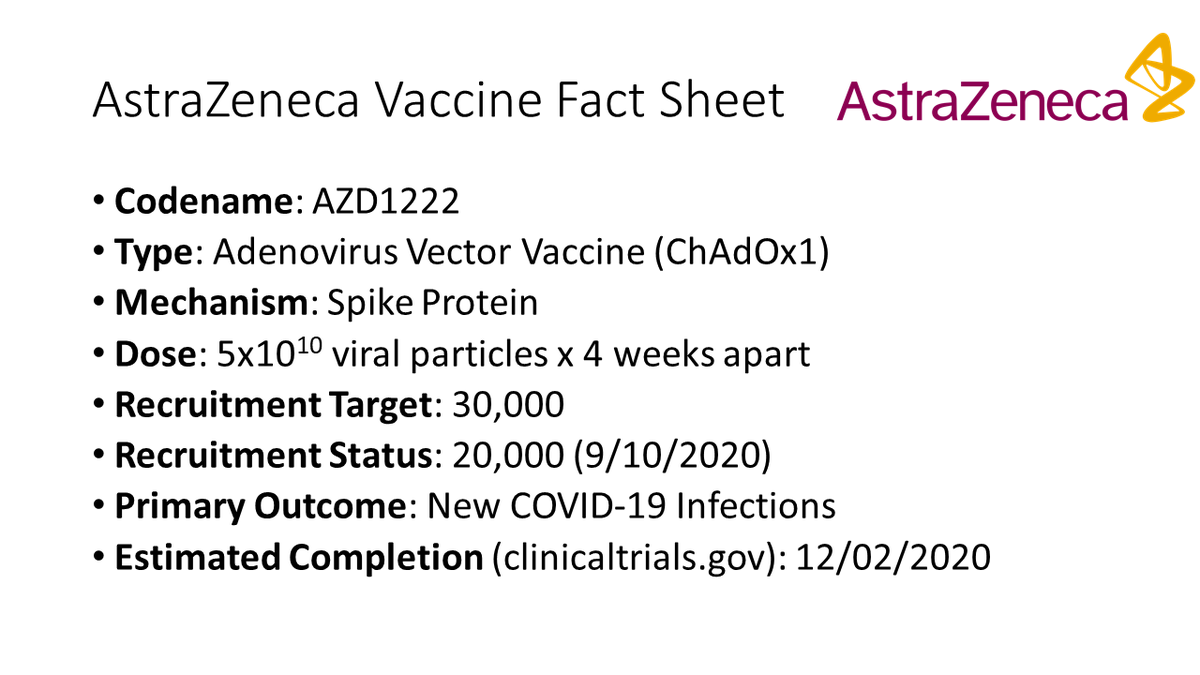
I have no idea which #vaccine
@realDonaldTrump was talking about today. But if we are going to have a vaccine before 2021, it will be one of these seven.
Here are the details (THREAD)
methodsman.com/blog/current-c…
@realDonaldTrump was talking about today. But if we are going to have a vaccine before 2021, it will be one of these seven.
Here are the details (THREAD)
methodsman.com/blog/current-c…
• • •
Missing some Tweet in this thread? You can try to
force a refresh