#OncoAlert Online now @ASCO_pubs - results from CheckMate 153 (continuous vs 1y fixed duration nivolumab for #NSCLC). This was a phase IIIB/IV study of salvage nivo monotherapy. Those with control at 1y were randomized to continue or stop. #LCSM @IASLC
ascopubs.org/doi/full/10.12…
ascopubs.org/doi/full/10.12…
252 patients were randomized and with a minimum f/u of 13.5m, mPFS strongly favored continuous over 1 year (mPFS 24.7 vs 9.4m, HR 0.56). The 1y PFS rate at 12m post-randomization was 65% if nivo continued (44% if stopped). We saw early PFS data at #ESMO17 presented by @dave6408. 

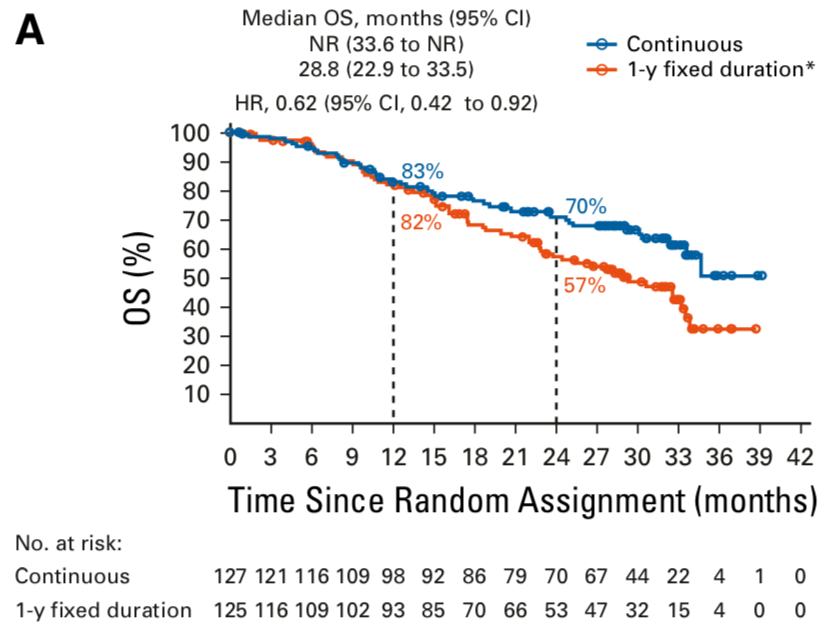
New to the #JCO @ASCO_pubs article are survival results. OS strongly favored continuous nivolumab over 1 year fixed dose (HR 0.62). While 1y OS rates were comparable, 2y OS rates were better with continues vs 1y fixed (70% vs 57%). #LCSM 
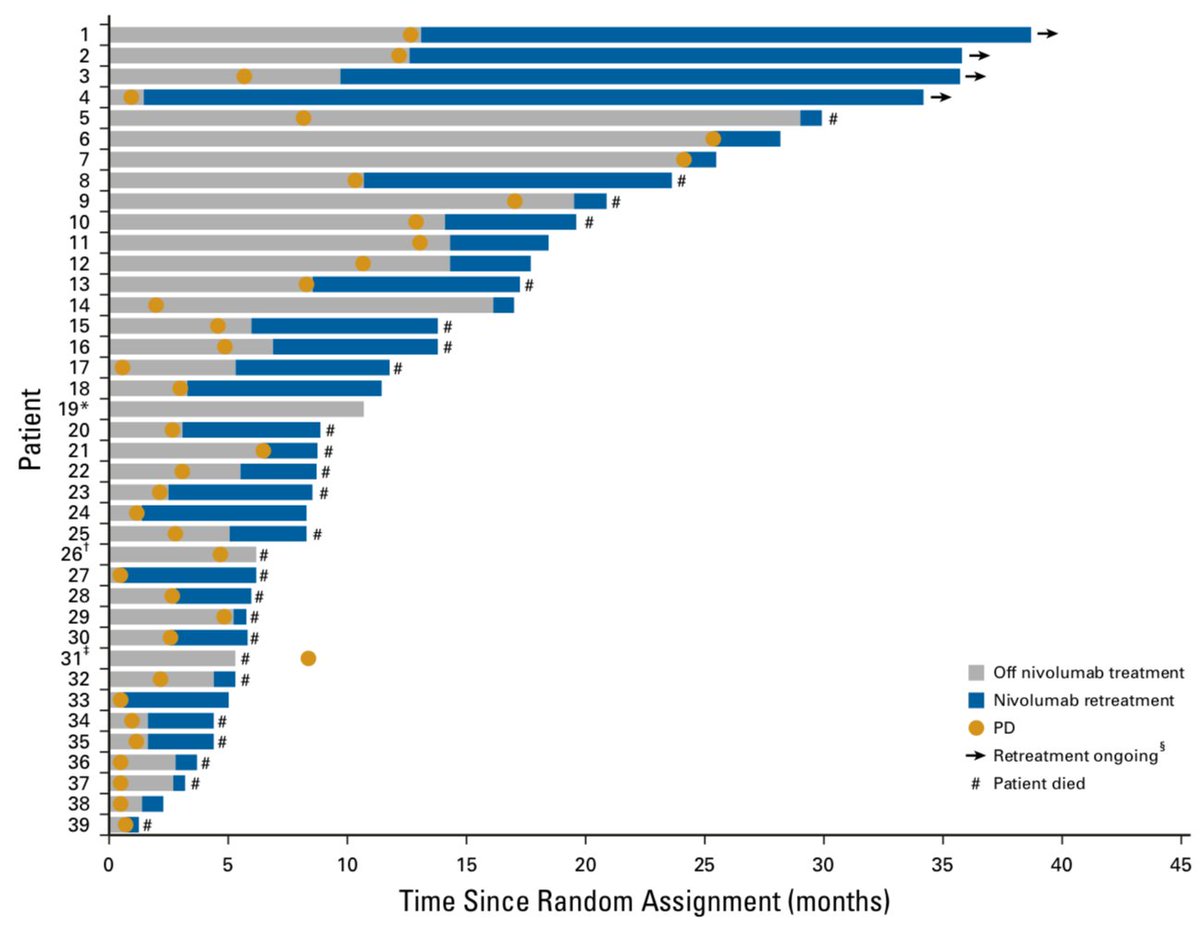
83% of those who stopped nivolumab at a year and progressed went on to restart nivolumab therapy. Responses were seen (dark blue in swimmers' plot below) and some quite durable but not all patients responded with a rechallenge. #LCSM 
CheckMate 153: 1y is not the preferred strategy for salvage nivolumab monotherapy. Continuous dosing improved PFS and OS but a different fixed point (2y) or a course tailored to specific tumor biomarkers may be preferred. Unclear if these trends would be the same in 1L setting. 

• • •
Missing some Tweet in this thread? You can try to
force a refresh