Our last paper is out: Left ventricular longitudinal shortening: relation to stroke volume and ejection fraction in ageing, blood pressure, body size and gender in the HUNT3 study openheart.bmj.com/content/7/2/e0…
I'll discuss some of the findings and their implications in a thread
I'll discuss some of the findings and their implications in a thread
2/ 1266 subjects without history of HT, heart disease or diabetes, LV linear measurements of systolic and diast. wall thickness, length, and diameters, entered into an ellipsoid LV model. 

3/ This gave us the possibility to look at age dependent changes in both volumes and functional measures, but with the two main limitations of the cross sectional nature of the study and for volumes the limitations of geometric model itself. There are still non-resolved issues.
Findings: Wall thickness increased, while LV length decreased with increasing age. FS was unchanged, while mAPSE decreased with age. LVEDV and SV both decreased, while EF was unchanged. 

There is still no consensus on which deformation component that contributes most to stroke volume;
circumferential shortening
pubmed.ncbi.nlm.nih.gov/23204893/
pubmed.ncbi.nlm.nih.gov/28818204/
Or longitudinal
pubmed.ncbi.nlm.nih.gov/11442577/
pubmed.ncbi.nlm.nih.gov/17098822/
circumferential shortening
pubmed.ncbi.nlm.nih.gov/23204893/
pubmed.ncbi.nlm.nih.gov/28818204/
Or longitudinal
pubmed.ncbi.nlm.nih.gov/11442577/
pubmed.ncbi.nlm.nih.gov/17098822/
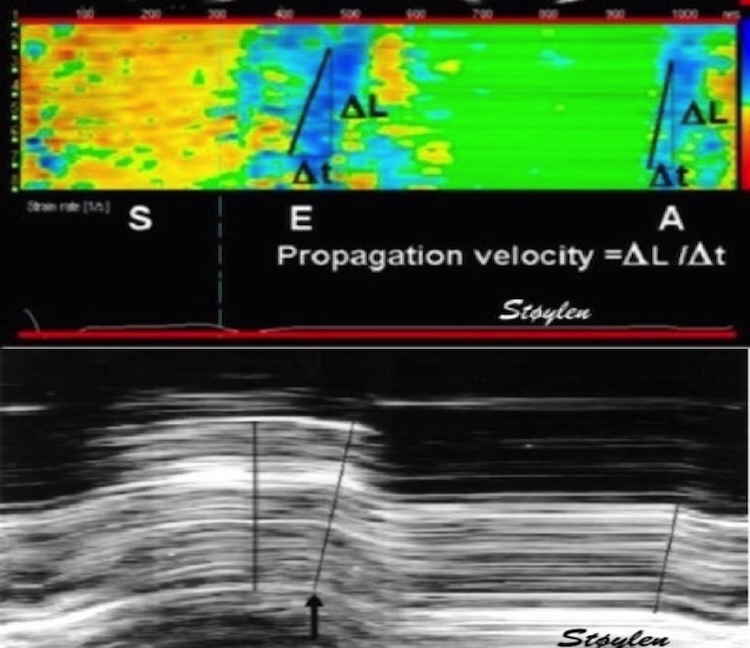
4/ If myocard is incompressible, myo volume doesn’t change in systole. Then volume decrease of the cavity (= SV), must equal volume decrease of total (outer) volume. Mitral annulus diameter is fairly constant, so the longitudinal SV component must be MAPSE x annular area. 

5/ In this study, SV calculated from EDV-ESV was 81.4ml, while Mitral area x MAPSE was 61.5 ml, = 74.2% of total SV. Circumferential shortening must make up the rest, 25.8%. @mugander 

Circumferential component is due to OUTER circ. (diameter) shortening, was 12.8%. Midwall or endocardial circ. shortening is not circ. fibre shortening, but mainly a function of wall thickening, which again is a function of wall shortening. 

6/ But is the myocardium truly incompressible? In this study we found a myocardial systolic compression of about 2.5% calculated as diff. between dias. and sys. myocardial volume. S/D Vol. ratio can in theory be calculated by (Sl + 1)(St + 1)(Sc+1), but not in practice.
Another issue is the (known) fact that MAPSE decreases with age, while EF is unchanged, so a compensatory increase in transverse (circumferential) function has been postulated, despite no studies have found increased FS, all have found it unchanged with age. What about this?
7/ No!. LVEDD unchanged, LV ED length decreases, ventricles get smaller and more spherical with age. Both LVEDV and SV decreases with age, so the ratio (EF) is stable. And the same with MAPSE; decreases with SV, so ratio remains const. No increased transverse function is needed 

Wall thickness increases by age, while LV length decreases. Does this mean that myocardial volume ("LV mass") increases or not? In this study, there was an increase in myocardial volume by age, from 101 to 114 ml.
8/ But despite selection for no known hypertension, there was increasing BP and no. of hypertensives with age. Corrected for BP, there was no independent effect of age on LV volume. @AnastasiaSMihai Seems HTN remains a factor in LVH even in the elderly. 

9/ But what about BP and MAPSE? Age and DBP were independently negatively correlated with MAPSE, SBP was not. So it seems that the modest increase in afterload did not give detectable effects on MAPSE @mariovar55 @load_dependent (offset by age effect?)
10/ #Cardiotwitter As pointed out by @mugander , there are limitations, both in the inherent over estimation by echo and in the ellipsoid model being symmetric, which LV is not. Thus the MAPSE fraction of 60% found by CMR pubmed.ncbi.nlm.nih.gov/17098822/ may be closer to the truth
11/ But systematic errors could be expected to be reasonably constant across age groups, sexes, BP groups and BSA, so the differences are the main object. And the study explains why MAPSE declines with age, while EF does not, without increase in short axis contraction
Unroll @threadreaderapp
• • •
Missing some Tweet in this thread? You can try to
force a refresh