Let’s talk about LDL and low carb diets.
🚨 THREAD FOR DOCTORS 🚨
Let’s first address the issues, you have no clue what you are looking at on a lipid panel.
Now since that’s out of the way, let’s let the education begin.
🚨 THREAD FOR DOCTORS 🚨
Let’s first address the issues, you have no clue what you are looking at on a lipid panel.
Now since that’s out of the way, let’s let the education begin.
The conventional medical knowledge is that LDL is causative for CVD.
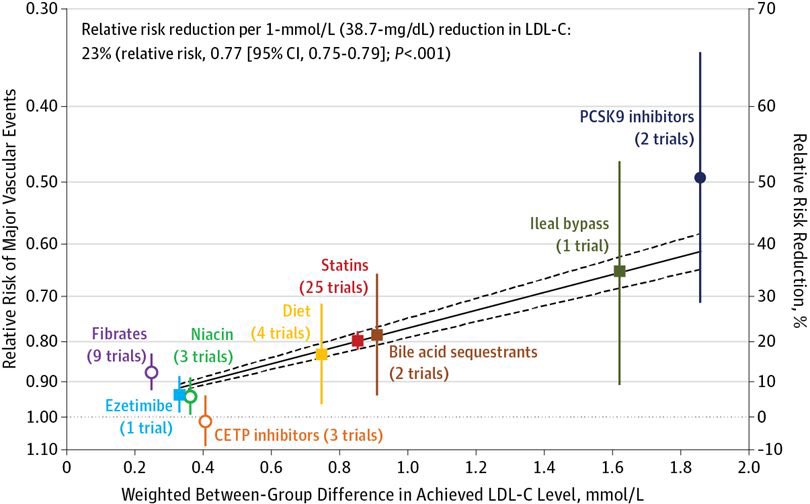
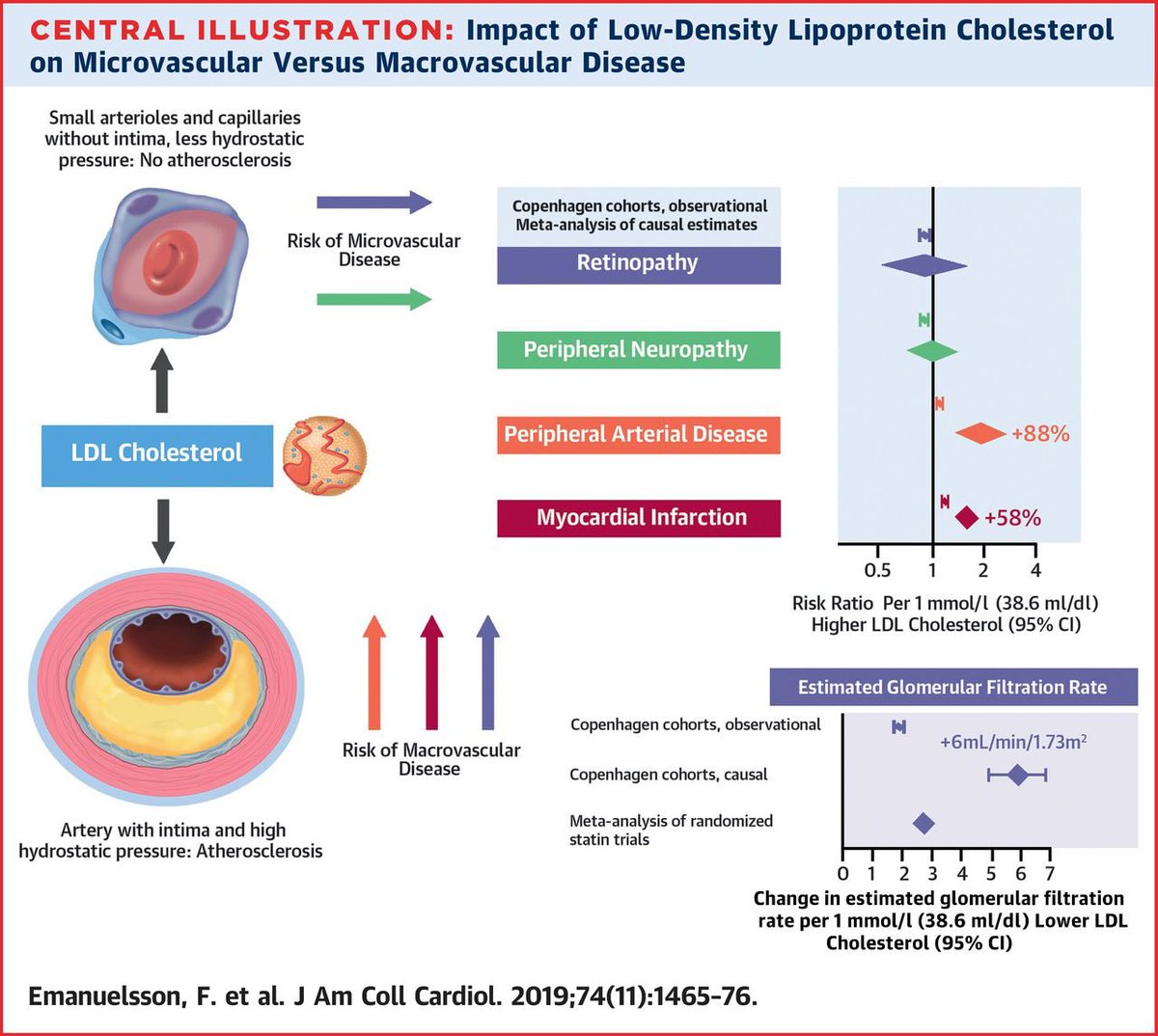
Many models have shown this, namely drug trials, Mendelian randomization, gene defect analyses and population association data
Many models have shown this, namely drug trials, Mendelian randomization, gene defect analyses and population association data
This is aggregated data from primary and secondary prevention trials
It appears that in both primary prevention there is a nominal improvement in CVD with LDL lowering whereas in secondary the benefit seems more robust
Nnt 200-500 in 1*
NNT 100-200 in 2*
It appears that in both primary prevention there is a nominal improvement in CVD with LDL lowering whereas in secondary the benefit seems more robust
Nnt 200-500 in 1*
NNT 100-200 in 2*
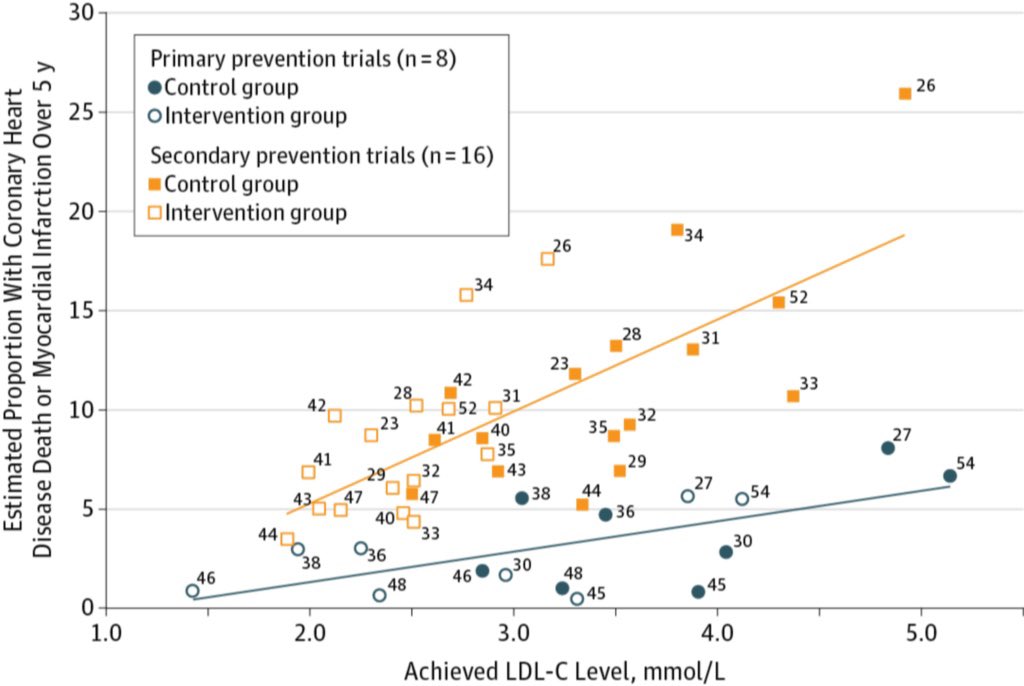
This is a strong case against a high LDL.
Unfortunately the common thinking is that LDL increase is caused by increased fat intake.
And to some extent that’s correct, but there are other factors to consider
Unfortunately the common thinking is that LDL increase is caused by increased fat intake.
And to some extent that’s correct, but there are other factors to consider
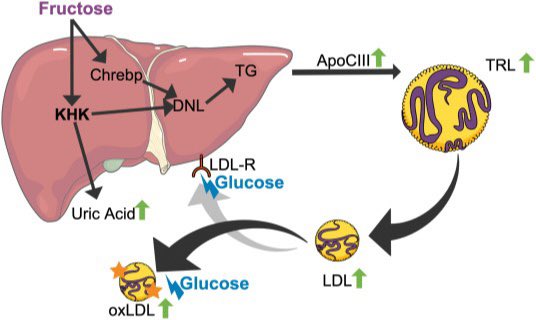
For example, LDL is also increased by fructose
Both in controlled feeding studies and real world clinical studies
academic.oup.com/jn/article/143…
sciencedirect.com/science/articl…
In fact glucose/fructose seem to be WORSE...
Both in controlled feeding studies and real world clinical studies
academic.oup.com/jn/article/143…
sciencedirect.com/science/articl…
In fact glucose/fructose seem to be WORSE...
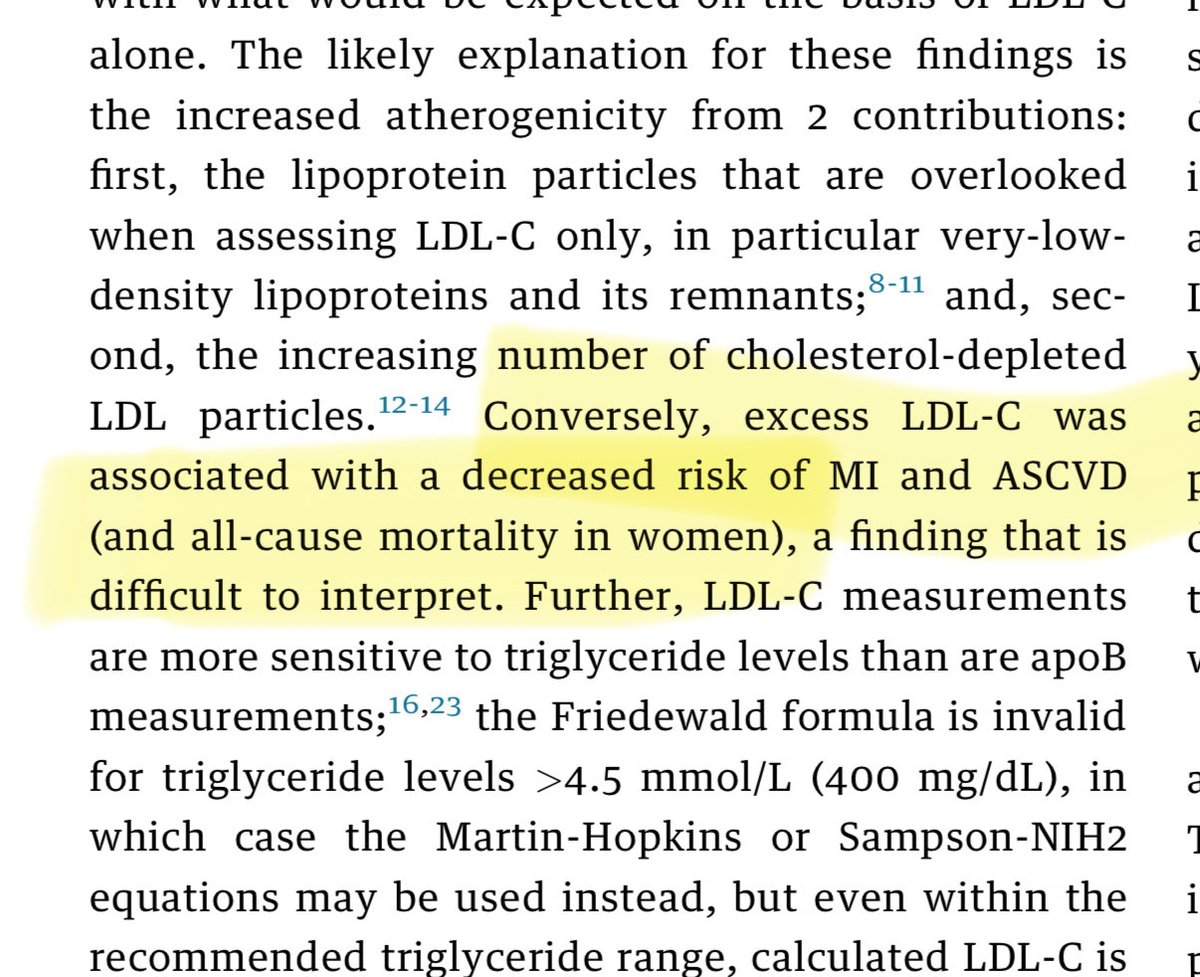
So as a patient with obesity and hyperinsulinemia begins a low carb diet there may be a reduction in LDL as the HLD of metabolic syndrome and fructose restriction comes into play...
But what happens as patients get leaner? Well there isn’t much data on long term low carb trials and certainly there isn’t much good data on the dyslipidemia of a population without metabolic syndrome
88% in the USA have one component of it... so what happens when you are free
88% in the USA have one component of it... so what happens when you are free
The lipid models for people who are not eating are VASTLY different than those who are eating.
IF during Ramadan causes an INCREASE in LDL
link.springer.com/article/10.100…
Anorexia increases LDL, refeeding DECREASES ldl...
pubmed.ncbi.nlm.nih.gov/19101189/
IF during Ramadan causes an INCREASE in LDL
link.springer.com/article/10.100…
Anorexia increases LDL, refeeding DECREASES ldl...
pubmed.ncbi.nlm.nih.gov/19101189/
I would be remiss if I didn’t discuss the amazing work of @DaveKeto in articulating and demonstrating the energy model that explain the low carb abs intermittent fasting lipid panel...
Basically when metabolic syndrome is resolved and triglycerides are low, if someone has lost or losing weight on low carb, I would EXPECT an increase in TOTAL, LDL and HDL cholesterol especially if TRF is also being practiced.
Unfortunately, many don’t know how to interpret these numbers. As evidenced by a recent thread by @MichaelMindrum @KCKlatt where general recommendations of lowering fat, swapping for PUFA/MUFA & increasing fiber were recommended.
While these interventions won’t likely worsen a lipid panel, and is a reasonable start, it will likely NOT effect the cholesterol numbers as they expect in these specific patients, particularly if over 250 LDL like was the case brought up by them.
I don’t blame them for thinking it would, if had mild early success with such interventions but it doesn’t last.
THE MOST RELIABLE way, from my clinical experience, to decrease LDL in such a case, is ADDING starch, increasing meal frequency &/or gaining fat mass.
THE MOST RELIABLE way, from my clinical experience, to decrease LDL in such a case, is ADDING starch, increasing meal frequency &/or gaining fat mass.
And since many are doing keto+IF for weight loss or maintenance, the reasonable option for many is to periodize starch to exercise and a modest amount in a second meal (separated from fat intake)
In the near future we will publish a small case series demonstrating this. But if you have followed @DaveKeto you could have expected the results. Massive decreases in LDL, amounts that are almost unfathomable.
To conclude this thread, I’d like to take this time and ask everyone to please donate to @DaveKeto charity. He will be putting your dollars to study these phenomena.
citizensciencefoundation.org/campaigns/lean…
citizensciencefoundation.org/campaigns/lean…
• • •
Missing some Tweet in this thread? You can try to
force a refresh