1/ Thread on myocardial work. What does it actually mean, and is it really useful? It is a spin-off from pressure-volume loops, which are an illustration to visualise the relation between stroke volume, pressure and contractility, and to assess physiology in animal experiments. 

2/ The area of the PV-loop is LV ejection work. The height of the PV-loop is the SBP-LVDBP difference, the width is the SV. Mean SBP and mean LVDBP ((blue dotted rectangle), shows the relation in an easy way. GMW is SV x (mean SBP - mean LVDBP). 

3/ This, of course means that it is definitely preload dependent, as increased preload increases SV. Increased afterload, on the other hand increases pressure work, but as afterload decreases SV, the relation is somewhat more uncertain. 

4/ Physiological experiments show pre- and afterload dependence of GMW. But GMW is not a measure of contractility, but LV energy expenditure. Contractility is the *ratio* of pressure and volume, roughly BP/SV, while work is the *product* of pressure and volume, roughly BP*SV 

5/ GLS, is a measure closely related to SV. Longitudinal shortening accounts for between 60 and 75% of SV, and this fraction seems to be fairly constant across ages and reduced function:
pubmed.ncbi.nlm.nih.gov/17098822/
openheart.bmj.com/content/7/2/e0… and
pubmed.ncbi.nlm.nih.gov/17098822/
openheart.bmj.com/content/7/2/e0… and

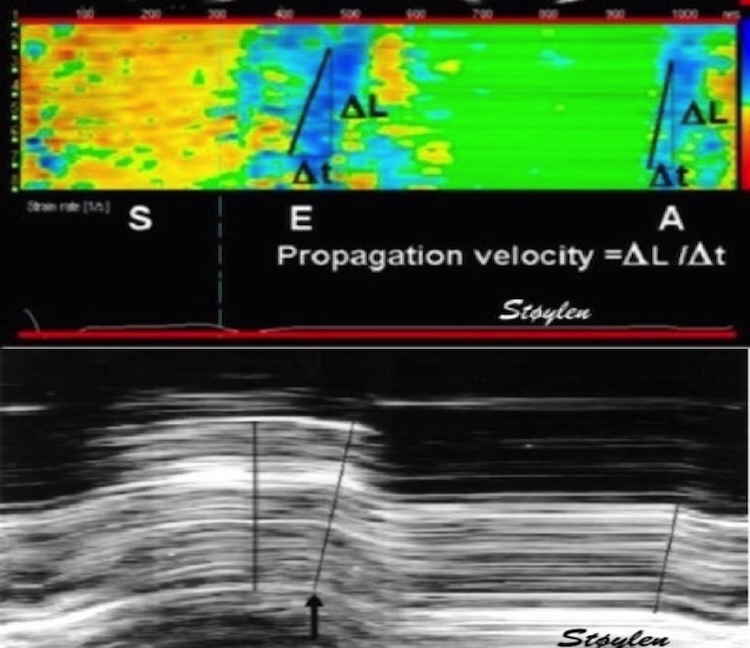
6/ Regional pressure strain loops are similar to global PV-loops, and shows regional oxygen consumption in animal experiments. pubmed.ncbi.nlm.nih.gov/7932236/.
7/ Using GLS and LV pressure gives a global pressure-strain loop; a proxy of true GMW. Longitudinal shortening contributes only a fraction to SV, this GMW proxy should be a fraction of the true GMW, although compensated somewhat by ST derived strain overestimating GLS somewhat. 

8/ Non-invasive pressure can be obtained from standardised pressure curve, time-calibrated by valve closures and openings, pressure calibrated by brach. cuff pressure. There is 1: No assessment of pressure augmentation and 2: LVDBP from a standard curve, is assumed normal. 

9/ It can still be valid for comparisons where these systematic errors may be assumed constant. But what does it mean physiologically, and what value clinically? Physiologically it is myocardial work (energy expenditure). But this increases by both output (SV) and load (demand)
10/ In an observational study, GMW correlated with both SBP and GLS, but a correlation between a compound measure and its components is hardly surprising. It
also correlated with SV, EF, MAPSE, and diastolic measures, also unsurprising.
pubmed.ncbi.nlm.nih.gov/31408147/
also correlated with SV, EF, MAPSE, and diastolic measures, also unsurprising.
pubmed.ncbi.nlm.nih.gov/31408147/
11/ In HFrEF, lower GMW predicted a poor prognosis, slightly better than GLS alone. pubmed.ncbi.nlm.nih.gov/32820318/ In this study, despite (lower) BP being significant in univariate analysis, it was taken out of the multivariate analysis.So then........
12/ But more hilarious: In a study of hypertension and diabetes, pubmed.ncbi.nlm.nih.gov/32966690/, GMW increased from normal to HT pts. (hardly surprising), and even more in pts. with HTR + diabetes, despite lower numerical GLS. So now, it seems that a *high* GMW is suddenly bad for you.
13/ So, it's not a measure of LV myocardial capacity, but a combination of performance and demand. Useful?......
But regional myocardial work was the start of it in the 70ies, it could probably be used to compare different regions of the LV. pubmed.ncbi.nlm.nih.gov/22315346/
But regional myocardial work was the start of it in the 70ies, it could probably be used to compare different regions of the LV. pubmed.ncbi.nlm.nih.gov/22315346/
14/ In this case, imitations of pressure curves are the same in all segments and do not matter. But so is the same with the pressure curve itself. It's the same pressure curve for all segments. So any difference in loops between segments, is only the difference in strain. 

15/ The width of the loop at AVC = end systolic strain, and with the same pressure input, all differences in loop shape and area are due to differences in regional strain. This is true whether this is due to schema, conduction, or other regional discrepancies. 

16/ But what about the wasted work concept? Wasted work can be seen in the strain - pressure loops, but has been demonstrated just as well by strain analysis alone, logical since only strain is different. pubmed.ncbi.nlm.nih.gov/22520537/
In my opinion, contractility is equivalent with supply (SV) vs demand (load = BP) - the ratio. Work is equivalent with supply x demand, what business finds this useful?
Unroll @threadreaderapp
• • •
Missing some Tweet in this thread? You can try to
force a refresh