I’ve not yet seen report on whether Trump has received dexamethasone (steroids); we know he already got remdesivir (antiviral) & “cocktail” of monoclonal antibodies.
But steroids, the only drugs proven to lower Covid mortality, raise a complex set of issues. An explainer. 1/9
But steroids, the only drugs proven to lower Covid mortality, raise a complex set of issues. An explainer. 1/9
The key is the dynamics of the immune system in Covid: early on, damage is being done by the virus itself, so rapid treatment w/ an antiviral & other efforts to bolster the immune response make perfect sense (although “making sense” & “proven to work” are 2 different things). 2/9 
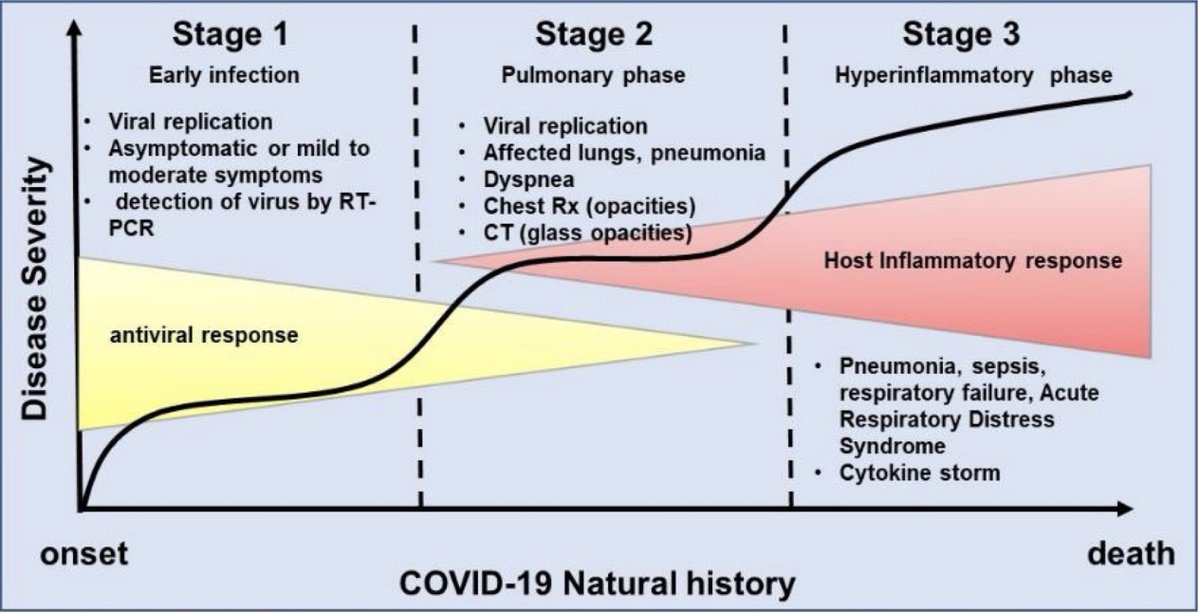
But steroids act differently – they suppress the immune system. Why could that work? Because later in Covid, some of the harm is by damage caused by our own immune systems going haywire – attacking our bodies in a frenzied effort to kill the intruder tinyurl.com/yyra4qnd 3/9
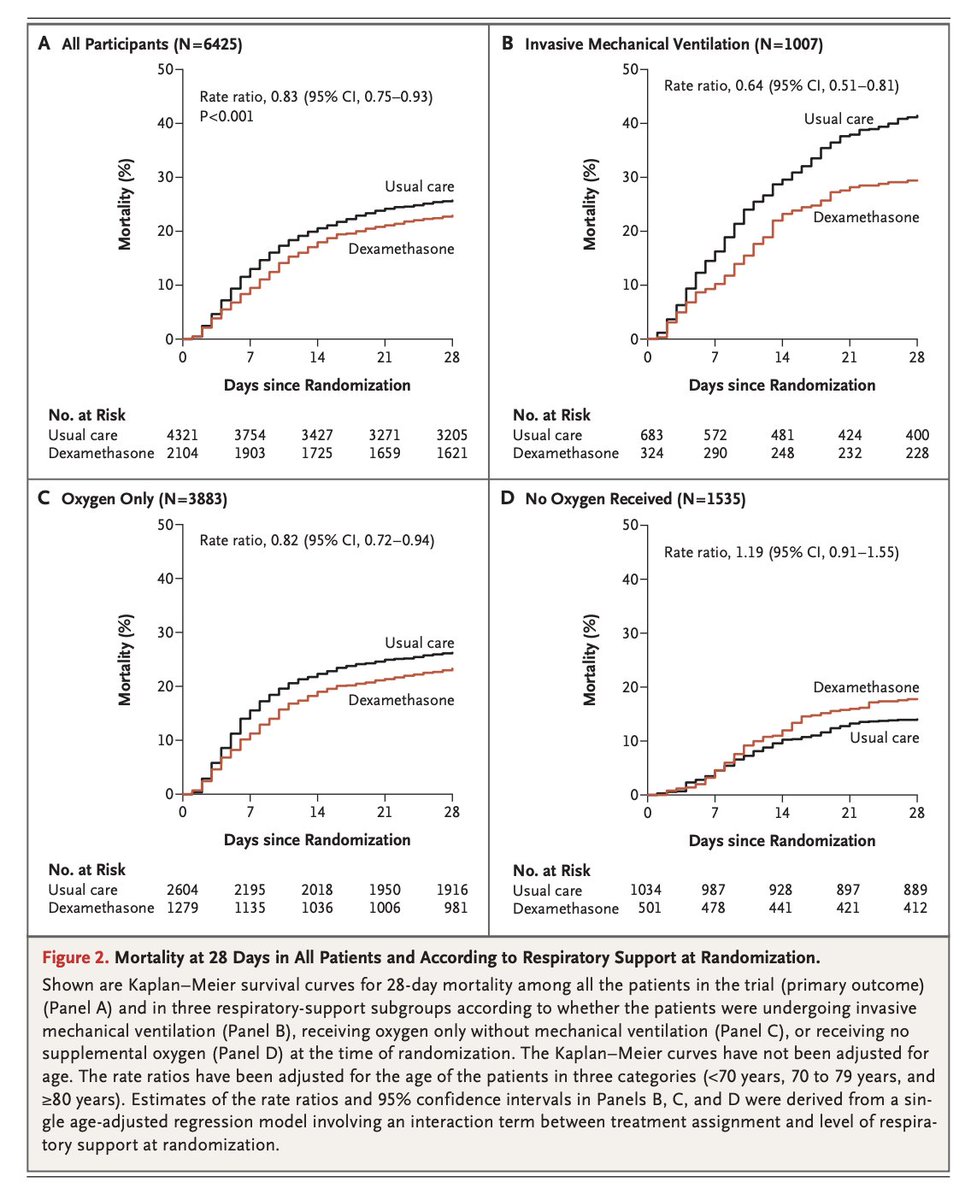
Because of that, one would NOT want to use steroids too early in the course of the illness. The trial proving benefit for steroids, the UK’s RECOVERY trial tinyurl.com/y3eqvuw8 randomized patients to dexamethasone or “usual care” at the time of admission to the hospital. 4/9
At randomization, 16% of patients were already on a respirator, 60% were on oxygen only, & 24% were receiving neither. If last night’s reports are to be believed, Trump would be in latter category. (Today’s medical briefing is at 11am Eastern, so hopefully we’ll learn more.) 5/9
Overall, dexamethasone reduced the probability of death by 17% (22.9% vs. 25.7% w/ usual care). Its greatest effects were in the group that required mechanical ventilation (29.3% vs. 41.4%), and those receiving oxygen but not on a mechanical ventilator (23.3% vs. 26.2%). 6/9
But in pts not on oxygen, dexameth. led to harm, though result wasn’t statistically signif. (17.8% w/ dex vs. 14.0% w/ usual care; Fig). These results argue that if, in fact, the president’s lung process is not far enough along to require oxygen, he should not be getting dex. 7/9 
Listen for this in the briefing. If Trump is not on oxygen & did get steroids, this may be an example of harmful VIP care: his receipt of antibodies on “compassionate use” isn’t unreasonable, though it hasn’t been approved. Nor was giving him IV remdesivir in the White House. 8/9
But, because it suppresses the immune system at a time when we want it to be working at full throttle, the use of dexamethasone in patients not yet requiring oxygen would constitute not only non-evidence based therapy, but one where evidence says it's likely to be harmful. 9/9
Sorry, a correction. Per his physician, his first dose of Remdesivir was given @WalterReedArmy, not in the White House 
• • •
Missing some Tweet in this thread? You can try to
force a refresh






