
1/ A🧵on the new Harrow et al paper "Twenty-year effects of antipsychotics in schizophrenia and affective psychotic disorders"
I really like the paper, and I try to make sense of it while avoiding uncritical acceptance as well as uncharitable rejection.
cambridge.org/core/journals/…
I really like the paper, and I try to make sense of it while avoiding uncritical acceptance as well as uncharitable rejection.
cambridge.org/core/journals/…
2/ It's remarkable that we have 20 yr follow-up data! This is extremely valuable for anyone interested in longitudinal course. It is important to however realize that it is a naturalistic study; subjects were not randomized to receive or not receive antipsychotics.
3/ This was a decision made by subjects/families/doctors in the course of their care (or lack of care) for a variety of possible reasons. These reasons are not known to us. Harrow et al are following the individuals and tracking the treatment they have received & their outcomes.
4/ The biggest mistake ppl make is to interpret the data from a naturalistic study as if it were an RCT; we cannot assume that the subjects in one group can be swapped with the subjects from the other group without changing the outcomes.
5/ So when the article says the odds ratio of not being on antipsychotics for those who achieved recovery was 6, it does *not* mean that a person can increase their chances of recovery 6x by no longer being on antipsychotic medication. That is an erroneous interpretation.
6/ Nonetheless, the results are striking, and Harrow et al do a great job trying to statistically control for as much as they can, including estimates of prognosis. This suggests that we need to take this study seriously; we cannot simply call it confounded and wash our hands.
7/ An important thing to note is that the sample size is still relatively small (n=139, n=70 for schizophrenia, 69 for bipolar)
8/ One finding it very clearly replicates is that 20% of ppl with schizophrenia do not experience further episodes of psychosis beyond their initial episode (an observation that goes back to Kraepelin) & long-term antipsychotic is likely unnecessary for these individuals
9/ However, the study suggests that even individuals who are not in that 20% group can still experience "recovery" (1 year symptom-free period with good functioning) & the likelihood of recovery seems to go up for individuals who are not receiving antipsychotic medications.
10/ 23% of subjects with schizophrenia were always psychotic, 20% never psychotic (after initial episode), and 57% intermittently psychotic (& they might be have transient periods of recovery) 
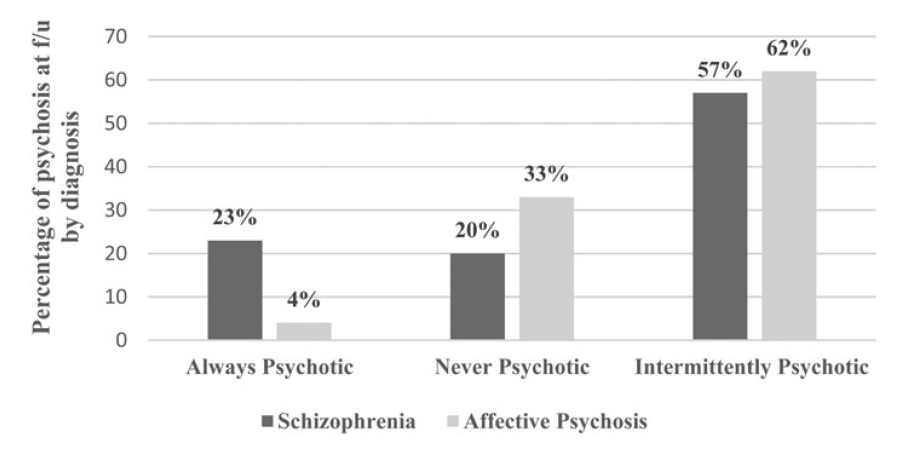
11/ Here we see a clear differentiation between schizophrenia and affective psychoses... if course of illness is a validator, this offers a partial validation of the distinction! 

12/ There is a tendency to think of antipsychotic use as a binary variable but this figure shows that's a simplistic view. A substantial portion of people were "intermittently prescribed" (presumably during acute exacerbations) 

13/ If some people achieve better outcomes with intermittent use of antipsychotics, that just suggests we may need to rethink how we approach long-term antipsychotic use, not that we need to abandon long-term use.
14/ Again, the sample size makes a difference. 25% of subjects with schizophrenia who were never prescribed antipsychotics is just 17 subjects. Hard to make grand conclusions with N=17.
15/ The biggest take home for me: we can't assume that everyone with schizophrenia needs to be on antipsychotics indefinitely; many will need to be, but that can't be the default expectation for everyone.
16/ For many, good outcomes are possible without the long-term use of antipsychotics. We should do what we can to determine if the patient in front of us could be one of those individuals.
• • •
Missing some Tweet in this thread? You can try to
force a refresh



