
1/
First of 2 tweets! #GalactoMagic
60M presents w/ 7 days of fevers & SOB. T 38.1C, HR 105, BP 110/70, RR 22, O2 95% on 6L & then intubated. Exam notable for diffuse crackles. CT chest shows GGO bilaterally. He has a +SARSCoV2 NAT resp swab; sputum & blood cultures are negative
First of 2 tweets! #GalactoMagic
60M presents w/ 7 days of fevers & SOB. T 38.1C, HR 105, BP 110/70, RR 22, O2 95% on 6L & then intubated. Exam notable for diffuse crackles. CT chest shows GGO bilaterally. He has a +SARSCoV2 NAT resp swab; sputum & blood cultures are negative
2/
After remdesivir, dexamethasone, ceftriaxone & doxy, he defervesces. 3 weeks later, he has worsening SOB. Repeat CT chest shows RUL cavitation. Serum BDG is 75 (positive>80) & serum GM is 0.4 (positive>0.5)
Which of the following diagnostics would have the highest yield?
After remdesivir, dexamethasone, ceftriaxone & doxy, he defervesces. 3 weeks later, he has worsening SOB. Repeat CT chest shows RUL cavitation. Serum BDG is 75 (positive>80) & serum GM is 0.4 (positive>0.5)
Which of the following diagnostics would have the highest yield?
1/13
Answer: BAL fluid culture
This patient is suffering from severe COVID-19 and is at risk for both bacterial and fungal super-infections
Although the most feasible test would be a sputum culture, the highest yield test for both bacteria and fungi is the BAL fluid culture
Answer: BAL fluid culture
This patient is suffering from severe COVID-19 and is at risk for both bacterial and fungal super-infections
Although the most feasible test would be a sputum culture, the highest yield test for both bacteria and fungi is the BAL fluid culture
2/
There are many causes of cavitary lung lesions
For this tweetorial, we will focus on a fungal super-infection after COVID-19, specifically, COVID-19-associated pulmonary aspergillosis (CAPA)
There are many causes of cavitary lung lesions
For this tweetorial, we will focus on a fungal super-infection after COVID-19, specifically, COVID-19-associated pulmonary aspergillosis (CAPA)
3/
CAPA pathophysiology is not completely understood, but may be 2/2:
🐶Viral effect on ciliary clearance
🐱Direct damage to airway epithelium
🐭Lymphopenia
🐹Viral effects on cellular-mediated immunity-?local and systemic immune paralysis
🐰Steroid use
pubmed.ncbi.nlm.nih.gov/33050499/
CAPA pathophysiology is not completely understood, but may be 2/2:
🐶Viral effect on ciliary clearance
🐱Direct damage to airway epithelium
🐭Lymphopenia
🐹Viral effects on cellular-mediated immunity-?local and systemic immune paralysis
🐰Steroid use
pubmed.ncbi.nlm.nih.gov/33050499/

4/
CAPA incidence ranges from 4-35%
This range is likely due to:
⚽️difficulty in diagnosis
🏀geographic & center differences
⚾️differences in CAPA definitions
🥎limited use & sensitivity of serum fungal markers
🎾varying rates of bronchoscopy
pubmed.ncbi.nlm.nih.gov/32887998/
CAPA incidence ranges from 4-35%
This range is likely due to:
⚽️difficulty in diagnosis
🏀geographic & center differences
⚾️differences in CAPA definitions
🥎limited use & sensitivity of serum fungal markers
🎾varying rates of bronchoscopy
pubmed.ncbi.nlm.nih.gov/32887998/
5/
CAPA is a disease entity seen in critically ill patients in the ICU
In addition to the reasons in tweet #4, CAPA can be difficult to diagnose because:
- it's hard to differentiate b/w colonization vs true pathogen
CAPA is a disease entity seen in critically ill patients in the ICU
In addition to the reasons in tweet #4, CAPA can be difficult to diagnose because:
- it's hard to differentiate b/w colonization vs true pathogen
6/
As we discussed before, distinguishing b/w infection and colonization requires consideration of:
🍏host vulnerability
🍎clinical signs & symptoms
🍐results of non-culture techniques (BDG, GM)
🍊radiographic findings
As we discussed before, distinguishing b/w infection and colonization requires consideration of:
🍏host vulnerability
🍎clinical signs & symptoms
🍐results of non-culture techniques (BDG, GM)
🍊radiographic findings
7/
Since RECOVERY, we've been using steroids in patients w/ COVID-19
It's unclear whether SARSCoV2 is the main RF for CAPA, or it’s a combination of factors including steroids & now tocilizumab
Steroids may be a RF for CAPA by blunting macrophage activity➡️fungal germination
Since RECOVERY, we've been using steroids in patients w/ COVID-19
It's unclear whether SARSCoV2 is the main RF for CAPA, or it’s a combination of factors including steroids & now tocilizumab
Steroids may be a RF for CAPA by blunting macrophage activity➡️fungal germination

8/
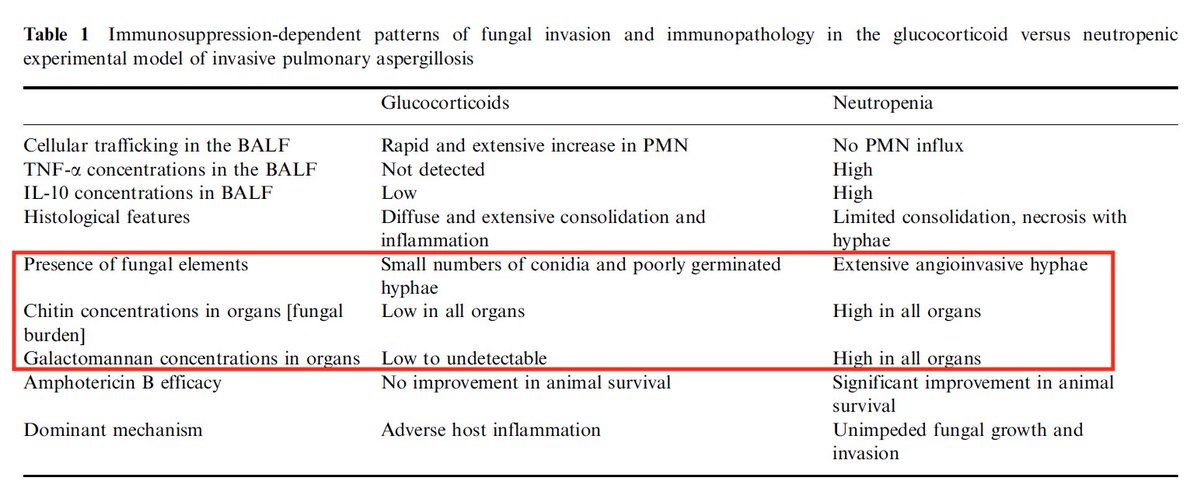
In neutropenic & steroid-treated mice models...steroid-associated aspergillosis had necrosis, less angioinvasion, & lower fungal burden
If this process is seen in CAPA, the lower fungal burden can affect our ability to detect fungus & GM
pubmed.ncbi.nlm.nih.gov/18654923/
In neutropenic & steroid-treated mice models...steroid-associated aspergillosis had necrosis, less angioinvasion, & lower fungal burden
If this process is seen in CAPA, the lower fungal burden can affect our ability to detect fungus & GM
pubmed.ncbi.nlm.nih.gov/18654923/
9/
We know that CAPA is an entity in pts that are critically ill in ICU. It’s diagnosed when:
🐺respiratory status worsens despite ARDS mgmt & ruling out other causes
🦝new, persistent, or rising fever while ruling out other causes
🦊progressive infiltrates, nodules/cavitation
We know that CAPA is an entity in pts that are critically ill in ICU. It’s diagnosed when:
🐺respiratory status worsens despite ARDS mgmt & ruling out other causes
🦝new, persistent, or rising fever while ruling out other causes
🦊progressive infiltrates, nodules/cavitation
10/
Why is it important for us to diagnose CAPA?
There have been several studies that have shown excess mortality rates of 16% & 25% compared with patients without evidence for aspergillosis
pubmed.ncbi.nlm.nih.gov/33333012/
Why is it important for us to diagnose CAPA?
There have been several studies that have shown excess mortality rates of 16% & 25% compared with patients without evidence for aspergillosis
pubmed.ncbi.nlm.nih.gov/33333012/
11/
Overall, diagnostic modalities include:
❤️Histopath examination of lungs
🧡Tracheal aspirates
💛BAL culture
💜Aspergillus PCR from BAL
💚Serum galactomannan (GM)
💙BAL galactomannan
🤎Serum beta-d-glucan
Overall, diagnostic modalities include:
❤️Histopath examination of lungs
🧡Tracheal aspirates
💛BAL culture
💜Aspergillus PCR from BAL
💚Serum galactomannan (GM)
💙BAL galactomannan
🤎Serum beta-d-glucan
12/
We can try to diagnose with sputum cultures, but their sensitivity in ICU pts for diagnosis of IPA does not exceed 50%, and we have previously reviewed the test characteristics of both serum and BAL GM in ICU patients
We can try to diagnose with sputum cultures, but their sensitivity in ICU pts for diagnosis of IPA does not exceed 50%, and we have previously reviewed the test characteristics of both serum and BAL GM in ICU patients
https://twitter.com/FilaMentor/status/1362817638292852738?s=20
13/
There are several proposed algorithms for diagnosing CAPA
Given how novel the disease entity is, it's difficult to come up with universal definitions
This algorithm is nice in that it provides helpful tips and different pathways with BAL vs no BAL
pubmed.ncbi.nlm.nih.gov/32703771/
There are several proposed algorithms for diagnosing CAPA
Given how novel the disease entity is, it's difficult to come up with universal definitions
This algorithm is nice in that it provides helpful tips and different pathways with BAL vs no BAL
pubmed.ncbi.nlm.nih.gov/32703771/

• • •
Missing some Tweet in this thread? You can try to
force a refresh



