Here's a 🧵summarizing my testimony on airborne transmission of COVID-19. Full version at edlabor.house.gov/hearings/clear… /0
COVID-19 is transmitted mainly by breathing in aerosol particles carrying the virus. Two other possible routes are 1) touching a sick person or contaminated object and 2) being sprayed by large respiratory droplets. These other routes are rarer. /1
Many cases of COVID-19 have been traced to “close contacts,” and this was incorrectly interpreted to mean that large droplets were responsible for transmitting the disease. /2
When people breathe, talk, sing, laugh, cough, or sneeze, they release far more aerosols than large droplets. These aerosols are most concentrated close to the sick person, and they don’t fall quickly to the ground. /3
When people talk in close proximity, it is much more likely that they will breathe in each other’s respiratory aerosols than shower each other with large droplets of spittle. /4
Aerosols remain floating in the air and follow air currents like cigarette smoke. Aerosols can easily travel more than 6 feet, filling a room and building up over time if the space does not have good ventilation. /5
Evidence for the importance of aerosol transmission includes superspreading events, transmission by people who are infected and don’t have symptoms (no coughing), much more indoor transmission and almost no outdoor transmission, various scientific studies. /6
If you spend a long time around other people indoors and do not wear a good mask, you could breathe in enough virus-containing aerosols to become sick with COVID-19. To limit exposure, avoid crowded indoor spaces and limiting time indoors with others. /7
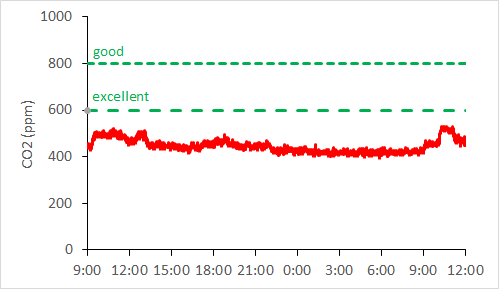
If contact with others cannot be avoided (e.g., essential workers), it is critical to reduce exposure to virus in the air by ensuring good ventilation—this reduces the amount of virus in the air—and wearing high-performance masks or respirators. /8
A worker who spends 8-12 hours in a poorly ventilated workplace where they share the air with other people is at much greater risk for transmission than a customer who passes through the space for a short period of time. /9
Face coverings work in both directions. They reduce the amount of virus that an infected person spreads into the air = “source control.” They can also reduce the amount of virus that the wearer breathes in from the air around them. /10
Some types of face coverings are much more effective than others against aerosols. The performance of a face covering depends on the filtration efficiency of the material and the fit. /11
Cloth masks have wildly varying filtration efficiencies of <10% to >90%. The actual performance also depends on fit. Leaks seriously degrade performance. /12
Surgical masks are good at filtration efficiency because they’re made out of meltblown, non-woven polypropylene, but bad at fit. /13
Respirators are designed to be tight fitting and to filter out aerosols with very high efficiency. Examples include N95s, KN95s, KF94s, elastomeric respirators. /14
For workers and others in high-risk settings, the hierarchy of controls calls for control of source (i.e., masking), engineering controls (i.e., ventilation and filtration), and PPE (i.e., high-performance masks or respirators). /15
Most CDC guidance and recommendations have not been updated or strengthened to address and limit inhalation exposure to aerosols. CDC downplays aerosols and airborne transmission, a position that is exactly opposite the best scientific evidence. /16
CDC’s FAQ on “How does the virus spread?”, emphasizes close contact and says nothing about inhaling the virus. /17
The Scientific Brief “SARS-CoV-2 and Potential for Airborne transmission” obfuscates by incorrectly equating all transmission at close proximity with droplets. This is wrong because transmission in close contact is dominated by inhalation of aerosols. /18
Why the reluctance? 1) Incorrect understanding of aerosols, 2) “airborne” has special meaning in hospitals, 3) concerns about limited supplies of N95s. /19
CDC must update and strengthen its guidelines to fully address transmission via inhalation of aerosols at both close distances and farther away. /20
Most CDC guidance and recommendations continue to emphasize distancing and surface cleaning, which are important, but less important than using high-performance masks and sufficient ventilation to clean the air. /21
Our letter (drive.google.com/file/d/1O5zd_J…) calls for CDC and OSHA to issue recommendations and requirements that address transmission of COVID-19 by inhalation of aerosols. /22
Calling the virus “airborne” is the clearest way to convey how it is transmitted. /23
This testimony is based on my 12+ years of studying viruses in the air and 30+ scientific papers on the subject, along with many discussions with colleagues (next tweet). Thanks to @jljcolorado @kprather88 for providing feedback on my testimony. /24
At the risk of overlooking some, especially newer ones: @Don_Milton Yuguo Li, Julian Tang, Lidia Morawska @Lakdawala_Lab @j_g_allen @ShellyMBoulder @CorsIAQ @CathNoakes Lydia Bourouiba @ProfCharlesHaas and all my students and post-docs! /25
• • •
Missing some Tweet in this thread? You can try to
force a refresh