
Thread 🧵
India should urgently change its COVID-19 vaccination strategy - why and how?
@MoHFW_INDIA @NITIAayog
(1/25)
India should urgently change its COVID-19 vaccination strategy - why and how?
@MoHFW_INDIA @NITIAayog
(1/25)
Change in strategy is not as simple as making vaccination open to all (vacc criteria).
Still after 35 days of phase II, the numbers suggest that the coverage among elderly is abysmal and this needs immediate correction
(2/25)
Still after 35 days of phase II, the numbers suggest that the coverage among elderly is abysmal and this needs immediate correction
(2/25)
Opening the vaccination to all will spread thin the already available doses. And it will also be an implementation nightmare.
This sounds fine at individual level but impractical and not correct at population level.
Again context specific exceptions could be made
(3/25)
This sounds fine at individual level but impractical and not correct at population level.
Again context specific exceptions could be made
(3/25)
During a pandemic in a developing country (cannot afford lockdowns) facing health worker fatigue, imperative that we quickly vaccinate the elderly (7% of pop) or if feasible >45y (22% of pop).
‘Quickly’ means attaining acceptable coverage within days/weeks, not months
(4/25)
‘Quickly’ means attaining acceptable coverage within days/weeks, not months
(4/25)
If we attain acceptable coverage among vulnerable now, the benefits of reduced hospitalisation will be observed after 6-8 weeks (time for immunity to set in followed by reduction in proportion with severe covid)
(5/25)
(5/25)
Health Information Technology (HIT, eg CoWin) should NOT be used at the cost of high coverage of vaccination, rapid pace of scale up and equity in coverage (which is happening now)
(6/25)
(6/25)
Currently it is mandatory to register in CoWin before vaccination.
Registration can be done by beneficiary a priori or post walk-in by the health care provider
(7/25)
Registration can be done by beneficiary a priori or post walk-in by the health care provider
(7/25)
Even walk-in requires a beneficiary to identify nearby facility that is a covid vaccination centre and on the day of walk-in slots should be available.
Here lies the uncertainty which may deter a common man
(8/25)
Here lies the uncertainty which may deter a common man
(8/25)
CoWin requires internet and is restricting vaccination upto primary health centres (PHC).
In many parts of the country, it takes around one day to go from home to PHC and return back to home.
Many PHCs may not even have good internet.
(9/25)
In many parts of the country, it takes around one day to go from home to PHC and return back to home.
Many PHCs may not even have good internet.
(9/25)
CoWin is centrally controlled and this includes approval of facilities as covid vaccination centres and the criteria for vaccination.
Software glitches and delays in receiving OTP are possible.
CoWin requires uploading ID proof details which again delays the process.
(10/25)
Software glitches and delays in receiving OTP are possible.
CoWin requires uploading ID proof details which again delays the process.
(10/25)
From time to time we come across guidelines (central Govt) that shows how detached our decision makers are from the ground reality.
For ex, at least half of the vaccinations should be through online apriori registration and rest may be through walk-in
(11/25)
For ex, at least half of the vaccinations should be through online apriori registration and rest may be through walk-in
(11/25)
Strategies that are used in public health should be simple enough for uniform implementation throughout the country.
Ideally strategies should be built upon existing mechanisms that are in place. This makes it easier for health system, health providers and beneficiaries
(12/25)
Ideally strategies should be built upon existing mechanisms that are in place. This makes it easier for health system, health providers and beneficiaries
(12/25)
CoWin dependent strategy is expecting people to visit facilities and get vaccinated.
For high and equitable coverage, we need to take the vaccines to the people.
In a pandemic, the onus should on the Govt to ensure that we attain high coverage
(13/25)
For high and equitable coverage, we need to take the vaccines to the people.
In a pandemic, the onus should on the Govt to ensure that we attain high coverage
(13/25)
Note that our public health vaccination system caters to 90% of routine immunisation.
We have successfully implemented vaccination campaigns in the past without private sector and internet/mobile App/web portals at the vaccination site
(14/25)
We have successfully implemented vaccination campaigns in the past without private sector and internet/mobile App/web portals at the vaccination site
(14/25)
Even in routine immunisation, if it were left only to people, the coverage would be lower than what we see.
Hence we have a combination of facility based vaccination along with outreach sessions at Anganwadi (usually once a month and at least once in three months)
(15/25)
Hence we have a combination of facility based vaccination along with outreach sessions at Anganwadi (usually once a month and at least once in three months)
(15/25)
I sincerely hope we shun CoWin, have a change in strategy and target vulnerable quickly through our public health vaccination system.
This will ensure wide coverage not only among urban well to do but also urban slums and rural areas (equity)
(16/25)
This will ensure wide coverage not only among urban well to do but also urban slums and rural areas (equity)
(16/25)
High and equitable COVID vacc coverage requires decentralisation all the way to the health sub-centre and Anganwadi.
There is NO NEED to collect individual level data.
There is NO NEED for a web portal (not every health worker has a smart phone, internet is an issue)
(17/25)
There is NO NEED to collect individual level data.
There is NO NEED for a web portal (not every health worker has a smart phone, internet is an issue)
(17/25)
Like pulse polio we may use indelible ink
First covid vacc dose can be indicated by the use of indelible ink on the left little finger (stays as long as 4 months in the nail cuticle).
The right little finger could be used for the second dose after one month
(18/25)
First covid vacc dose can be indicated by the use of indelible ink on the left little finger (stays as long as 4 months in the nail cuticle).
The right little finger could be used for the second dose after one month
(18/25)
Microplans, trainings, logistics, IEC/BCC and community participation shld be ensured (using our experience from pulse polio / measles SIA campaign).
WHO NPSP consultants (involved in routine immunisation) may provide technical support
(19/25)
WHO NPSP consultants (involved in routine immunisation) may provide technical support
(19/25)
Primary health centres (PHC) should be the nodal point to serve a designated population and generate data.
Cumulative Vaccine coverage data (numerator and estimated denominator) may be shared bottom up.
This same mechanism may also be used to report AEFI.
(20/25)
Cumulative Vaccine coverage data (numerator and estimated denominator) may be shared bottom up.
This same mechanism may also be used to report AEFI.
(20/25)
The above data (called as health management information system HMIS data) could be filled in an online HMIS portal at PHC.
Similar mechanism is followed to generate HMIS data for our primary health care services provided by public health system
(21/25)
Similar mechanism is followed to generate HMIS data for our primary health care services provided by public health system
(21/25)
Keeping in mind the local context and situation, manpower and expertise, the states should have the freedom to modify criteria and strategy
For ex large states may use a sectoral approach (big cities first and then rest)
Small states may target all eligible at one go
(22/25)
For ex large states may use a sectoral approach (big cities first and then rest)
Small states may target all eligible at one go
(22/25)
It is OK for states to have different strategies and criteria.
Even within a state/district, Urban PHCs’ microplan may be different from Rural PHCs.
Media and public should not deride this.
Centre should visibly play a supportive role
(23/25)
Even within a state/district, Urban PHCs’ microplan may be different from Rural PHCs.
Media and public should not deride this.
Centre should visibly play a supportive role
(23/25)
High level state and centre officials should hold joint press conf and update what is being done and why (take questions). If required this should be done by PM and CM.
Image of a leader is NOT more important than lives of people
(24/25)
Image of a leader is NOT more important than lives of people
(24/25)
This should be complemented with a positive campaign for masking (on the lines of theory of diffusion of innovation).
Utmost care should be taken that existing health services and health programmes (including routine immunisation) are not affected.
🙏🏻
(25/25)
Utmost care should be taken that existing health services and health programmes (including routine immunisation) are not affected.
🙏🏻
(25/25)
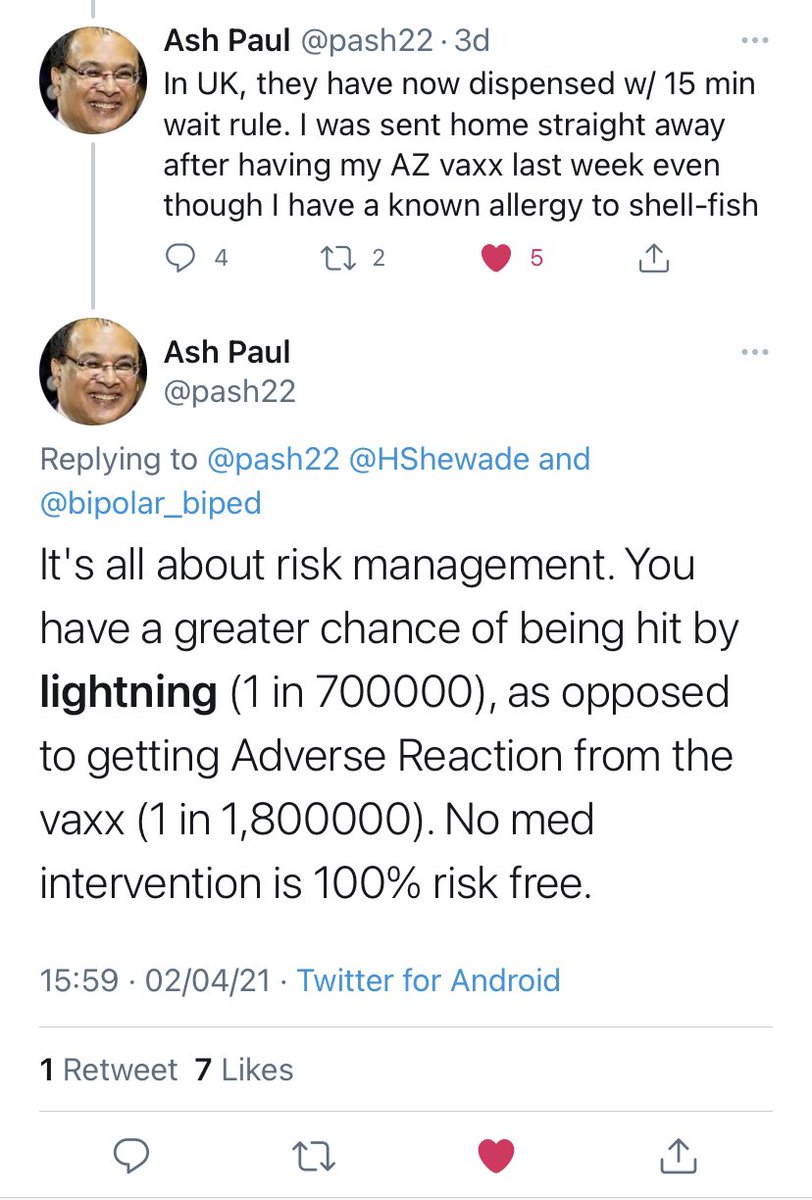
Reg AEFI immediately after vaccination, look what other countries are doing 👇
Why can’t AEFI be monitored and reported the way we do in our public health vaccination programme. What has this covid vacc AEFI monitoring in India achieved till now?
Why can’t AEFI be monitored and reported the way we do in our public health vaccination programme. What has this covid vacc AEFI monitoring in India achieved till now?
• • •
Missing some Tweet in this thread? You can try to
force a refresh


