I know we are all applauding @JoeBiden for his response to India today, but, to be honest, I think Biden's response is actually really bad. And it shows that nearly 100 days into his administration, they still don't have a plan for ensuring global vaccination. 🧵
First, as @zainrizvi has pointed out, the WH was clear that the materials that would be sent to Serum Institute of India would be for Covishield (the SI version of AZ/Oxford). The only problem? There was NO materials shortage for Covishield that was inhibiting production. 

Instead, @SerumInstIndia cannot access supplies for the OTHER COVID-19 vaccine it produces, Covovax, their version of @Novavax, *and not Covishield*. Serum Institute has been 100% explicit about this (once again h/t @zainrizvi):
https://mobile.twitter.com/SaketGokhale/status/1386173220445986826
Is this a mistake @JakeSullivan46? But regardless, we have seen nothing from the administration on how the US is going to scale manufacturing capacity for both raw materials and consumables (biorx bags, filters/columns etc,) necessary for scaling up vaccine production globally.
In fact, the administration has had US$10 BILLION, authorized by the COVID rescue package, to do exactly this since MARCH, and yet has to done nothing. congress.gov/bill/117th-con… 

And the Bio E investment announced today is similarly unambitious -- 1 billion doses (enough to cover 700 million people) by end of 2022(!), is too little, too late. And remember 600 million doses of that capacity is for a vaccine that has yet to even enter phase 3 trials.
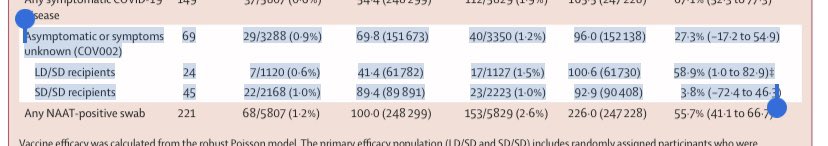
So we are scaling capacity for a vaccine that we don't even knows works, all while the Biden Administration has refused to explain why @Novavax candidate has still not even be authorized, despite posting excellent phase 3 results in January.
• • •
Missing some Tweet in this thread? You can try to
force a refresh