
Why that @prof_tweet modelling paper does NOT show that online triage increases GP workload, and what we can learn from it. THREAD⬇️
@MinalBakhai @HelenRSalisbury @padsbigsis @mgtmccartney @keithgrimes @MartinRCGP @murrayellender @fhussain73 @bcdelaney1 @BenXGowland @ClareGerada
@MinalBakhai @HelenRSalisbury @padsbigsis @mgtmccartney @keithgrimes @MartinRCGP @murrayellender @fhussain73 @bcdelaney1 @BenXGowland @ClareGerada
https://twitter.com/prof_tweet/status/1389996243087249414
I preface this by saying @prof_tweet is great and his 2018 Mackenzie lecture profoundly influenced my thoughts on general practice.
spcr.nihr.ac.uk/news/james-mac…
spcr.nihr.ac.uk/news/james-mac…
As the paper acknowledges, the benefits/costs of online triage depend strongly on the assumptions fed into the model.
There is one HUGE assumption that, on its own, makes the difference between huge efficiency and huge inefficiency.
There is one HUGE assumption that, on its own, makes the difference between huge efficiency and huge inefficiency.
This assumption is not explicitly acknowledged in the paper. It can't be tweaked in the online calculator. I had to reproduce the model myself to realise they had made this assumption.
An encounter managed purely online is assumed to take 4 mins. Fine.
But they add these 4 minutes to *every* consultation, including the 80% resolved by phone and/or F2F.
In the model, these 4 minutes are wasted. They don't save time in the subsequent phone call / F2F.
But they add these 4 minutes to *every* consultation, including the 80% resolved by phone and/or F2F.
In the model, these 4 minutes are wasted. They don't save time in the subsequent phone call / F2F.
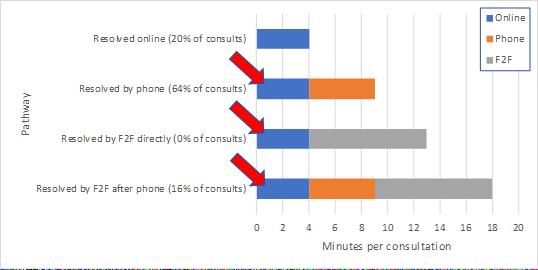
This - what to call it? - "triage time" is catastrophically inefficient. Under their base case, 34% - ONE THIRD - of all GP time is spent on this online step for contacts that go on to require phone/F2F.
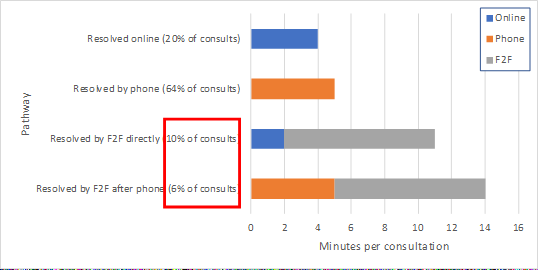
Simply reducing this "triage time" to reasonable levels is enough to reverse the conclusion: rather than being 9% less efficient than conventional care, online triage becomes 28% MORE efficient. 

The only evidence for this "triage time" seems to come from a 2015-16 study in which e-consultation use was negligible (and so the pathway was hardly likely to be optimal) and the triage time was not actually measured. 


🩺 Clinical tip 1: the triage step needs to be rapid. Make a quick decision about whether the consultation is best resolved via online, phone or F2F. Use tech or receptionists (or both together) to make the easy decisions (e.g. F2F for new breast lump).
It's also odd that the updated @prof_tweet base case assumes that no patient gets F2F without a call first. A big benefit of online triage is the written history which allows the GP, in many cases, to predict a F2F is required and skip the phone step.
If we assume instead that the phone step is skipped for 60% of F2F encounters, while keeping total F2F proportion at 16%, the efficiency advantage of online triage goes up again to 32%. 
🩺 Clinical tip 2: it's online triage, not phone triage. You don't need to phone everyone. If you can tell from the online form that F2F will probably be required, go straight to F2F. Play the probabilities.
🩺 Clinical tip 3: if F2F is needed after a phone call, it should be done by the same clinician. Otherwise the history-taking will be repeated. Do the F2F on the same day while the history is fresh in your mind.
If I plug in real outcome data for clinicians at my practice over the last month (42% online, 41% phone, 17% F2F), the efficiency advantage of online triage is around 33%. 

Now, I don't put any faith in that 33% stat. I don't claim to have shown that online triage is any more efficient than the conventional model. Rather, there is far too little evidence to make any conclusion, and it's *plausible* that online triage can be more efficient.
Lastly: we need a stronger relationship between academics like @prof_tweet and the innovators in the NHS. Too often an intervention is rolled out after a pilot and a flimsy "evaluation" that wouldn't get past peer review.
But we need to avoid killing off promising ideas by pronouncing judgement based on insufficient evidence, or before the new way of working has had a chance to mature.
If we gave up on ideas just because they didn't work well at the first attempt, we would have missed out on many huge advances, such as mRNA vaccines.
statnews.com/2020/11/10/the…
statnews.com/2020/11/10/the…
As I've said before, the triage model is just getting started and it's hard to argue that it won't one day be far superior to the conventional model.
https://twitter.com/EdTurnham/status/1377738866422075395?s=20
• • •
Missing some Tweet in this thread? You can try to
force a refresh



