1/ I know some of us have already had a brief discussion about this, but this is the most astonishing presentation I have seen in a long time.
We should discuss!
I must stress, I have *not* seen the actual presentation, I've seen the slides & write up on TCTMD only
We should discuss!
I must stress, I have *not* seen the actual presentation, I've seen the slides & write up on TCTMD only

2/ This study is derived from the TVT registry, looking at TAVIs with the Sapien 3/Ultra between 2015-2020
Of 159661 TAVIs, 37660 were in low risk patients (STS score <3%) & 3243 had bicuspid AV. They've propensity score matched to compare TAVI in BAV vs trileaflet AV valves
Of 159661 TAVIs, 37660 were in low risk patients (STS score <3%) & 3243 had bicuspid AV. They've propensity score matched to compare TAVI in BAV vs trileaflet AV valves

3/ Almost all the BAV pts made it into the propensity score-matched group (3168/3243 = 97.7%)
Mean age 69yrs
Mean STS score 1.7%
Mean LVEF 57%
Mean age 69yrs
Mean STS score 1.7%
Mean LVEF 57%

5/ This is an important slide
At 1yr, the mortality in the group with trileaflet aortic valves was 6.6%
6.6%. Think about that. *Low-risk* cohort. Mean age 69.
PARTNER 3 1yr mortality? 1%
At 1yr, the mortality in the group with trileaflet aortic valves was 6.6%
6.6%. Think about that. *Low-risk* cohort. Mean age 69.
PARTNER 3 1yr mortality? 1%

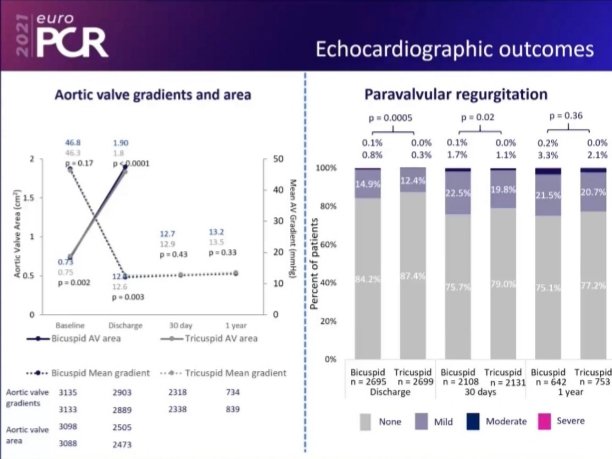
6/ More outcomes here
Pts with BAV were more likely to need re-intervention within 1yr than those with tricuspid AV (1.16% vs 0.43%)

Pts with BAV were more likely to need re-intervention within 1yr than those with tricuspid AV (1.16% vs 0.43%)

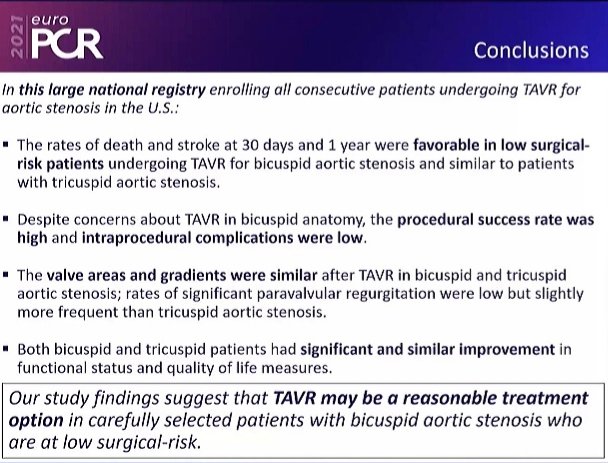
7/ The conclusion slide is a masterclass in spin
It's insightful how they've chosen to focus on certain aspects of the data & completely ignore other aspects
It's insightful how they've chosen to focus on certain aspects of the data & completely ignore other aspects
8/ Here, I've created a possible alternative Conclusions slide!
Negative spin, I hear you say!
But, still in line with the data presented, yes?
Surely the right approach is somewhere in between these 2 extremes?
Negative spin, I hear you say!
But, still in line with the data presented, yes?
Surely the right approach is somewhere in between these 2 extremes?

9/ The presentation was covered in detail by @ToddNeale for @TCTMD - a great write-up with lots of detail from Todd...but I can't agree with the positivity in the title or lack of a counterview in the article!
Even more alarming, a hint RCTs not needed?

Even more alarming, a hint RCTs not needed?


10/ Final thoughts?
1. Amazed that TAVI in BAV in younger, low risk pts is taking place (yes, even in 🇺🇸) without any proper evidence that it's the right thing to do, or equivalent to surgery. In the absence of such data, would love to know how ICs consented these patients...
1. Amazed that TAVI in BAV in younger, low risk pts is taking place (yes, even in 🇺🇸) without any proper evidence that it's the right thing to do, or equivalent to surgery. In the absence of such data, would love to know how ICs consented these patients...
11/
Look at how different real-world TAVI outcomes are compared to the strictly controlled environment of a RCT...6.6% mortality at 1yr in low-risk patients. Just dreadful.
Admittedly we don't know causes of death, but it's so much worse than trial data
Look at how different real-world TAVI outcomes are compared to the strictly controlled environment of a RCT...6.6% mortality at 1yr in low-risk patients. Just dreadful.
Admittedly we don't know causes of death, but it's so much worse than trial data
12/
The spin on the final slide is depressing. That's the best word for me. It's disingenuous to ignore the other points that merit discussion. And to suggest this can now be done in select patients...? No! We did trials that excluded these pts for a reason
Now we study them...
The spin on the final slide is depressing. That's the best word for me. It's disingenuous to ignore the other points that merit discussion. And to suggest this can now be done in select patients...? No! We did trials that excluded these pts for a reason
Now we study them...
13/ Finally. I'm an imaging cardiologist, neither IC nor surgeon so I'm not favouring one over another. I favour being honest & doing things the right way, and this doesn't sit well with me. At all
Would love to know what you all think. But - ICs & surgeons - keep it civil! 😁
Would love to know what you all think. But - ICs & surgeons - keep it civil! 😁
14/ PS - usual caveat. I'm not a luddite! Not anti-Industry or anti-progress. I run our @UHS_valveclinic from which I refer patients for TAVI consideration almost every week.
I think it is possible to be pro-innovation and pro-proper science at the same time
#cardiotwitter
I think it is possible to be pro-innovation and pro-proper science at the same time
#cardiotwitter
• • •
Missing some Tweet in this thread? You can try to
force a refresh