Ivermectin proponents point to in vitro studies as proof of efficacy
One problem: the dose required in vitro (IC50) to inhibit #COVID is 30-90x higher than the plasma or tissue levels (Cmax) achieved with a standard 12mg IVM dose
A 🧵 explaining & debunking this myth
1/
One problem: the dose required in vitro (IC50) to inhibit #COVID is 30-90x higher than the plasma or tissue levels (Cmax) achieved with a standard 12mg IVM dose
A 🧵 explaining & debunking this myth
1/
First some definitions:
- Cmax is the maximum concentration achieved after a medication is given; it is usually measured in healthy people
- IC50 is the concentration of a drug necessary to inhibit a particular enzyme or process by 50%; it is measured in vitro.
2/

- Cmax is the maximum concentration achieved after a medication is given; it is usually measured in healthy people
- IC50 is the concentration of a drug necessary to inhibit a particular enzyme or process by 50%; it is measured in vitro.
2/


Since the pandemic began, many studies looked at repurposing FDA approved drugs to treat COVID
Literally dozens of candidate drugs have been found that inhibit viral replication in vitro
One of these candidates is ivermectin
But as we will see the devil is in the details...
3/


Literally dozens of candidate drugs have been found that inhibit viral replication in vitro
One of these candidates is ivermectin
But as we will see the devil is in the details...
3/


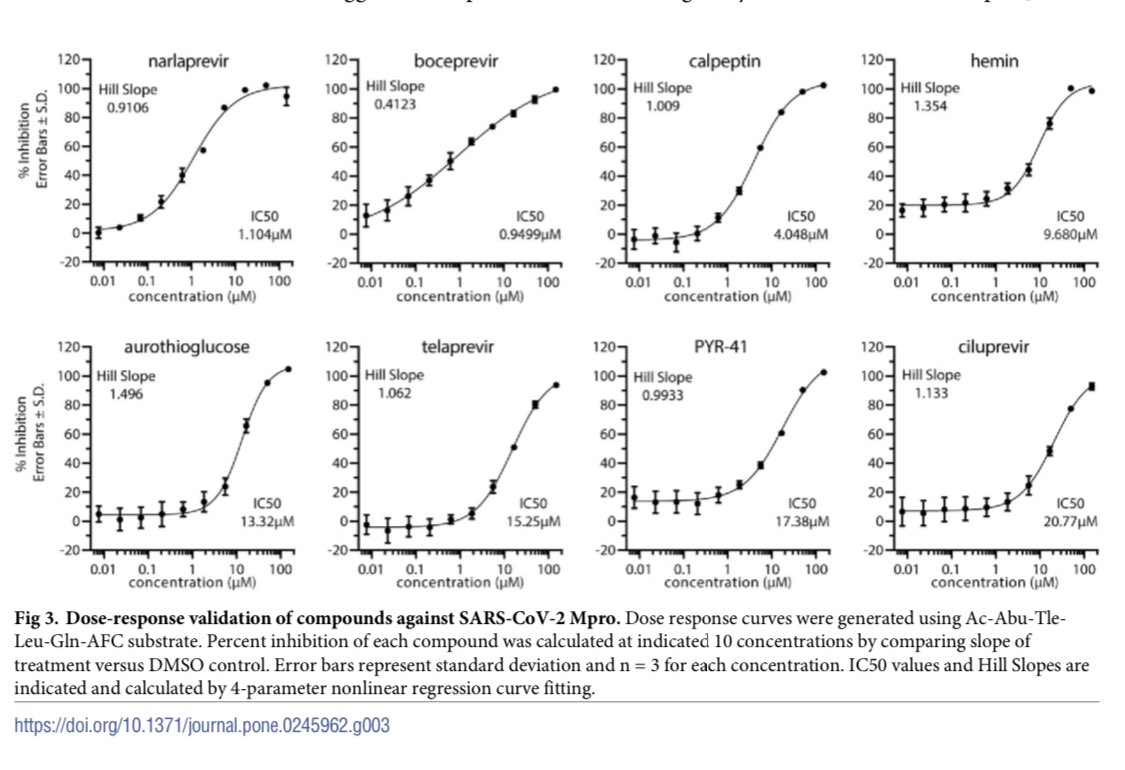
The key study by Caly et al found that at a concentration of 5 μM ivermectin inhibited SARS-CoV-2 replication (IC50) in Vero cells (African Green Monkey Kidney cells)
🐒 kidney cells aren’t exactly proof of efficacy in humans but this is promising
Except there’s a problem...
4/

🐒 kidney cells aren’t exactly proof of efficacy in humans but this is promising
Except there’s a problem...
4/


...the dose that inhibits SARS-CoV2’s replication (IC50) in vitro is MUCH higher than the concentration of ivermectin (Cmax) that’s actually achieved in humans taking the highest dose of the drug:
IC50 5 μM
vs
Cmax 0.05 μM (on 200 mcg/kg)
That’s 100x less drug than needed!
5/
IC50 5 μM
vs
Cmax 0.05 μM (on 200 mcg/kg)
That’s 100x less drug than needed!
5/
Ivermectin proponents argue that the drug accumulates in lungs & therefore reaches an effective level.
This too has been debunked in this excellent paper by Schmith et al👇
medrxiv.org/content/10.110…
6/
This too has been debunked in this excellent paper by Schmith et al👇
medrxiv.org/content/10.110…
6/

Using measurements from cow lungs & serum, they calculate the tissue distribution of ivermectin.
Even though Cmax was higher for lung (0.08 μM vs 0.05 μM) it was still much less than the IC50 needed to inhibit SARS-CoV2 (5 μM).
That’s still 62x too low to be effective!
7/

Even though Cmax was higher for lung (0.08 μM vs 0.05 μM) it was still much less than the IC50 needed to inhibit SARS-CoV2 (5 μM).
That’s still 62x too low to be effective!
7/


What if we just use a 10x higher dose of Ivermectin (e.g. 120 mg instead of the standard 12 mg)?
We still come up well short!
Even at this dangerously high 10x usual dose, our lung specific Cmax is only 0.8 μM compared to an IC50 of 5 μM (still 6x too low to be effective).
8/

We still come up well short!
Even at this dangerously high 10x usual dose, our lung specific Cmax is only 0.8 μM compared to an IC50 of 5 μM (still 6x too low to be effective).
8/


This brings us to another key point: toxicity.
Ivermectin proponents argue that the drug is safe & widely used. This is true, in healthy outpatients treated with a low *weekly* dose.
Critically ill inpatients on a high *daily* dose are much more likely to develop toxicity.
9/
Ivermectin proponents argue that the drug is safe & widely used. This is true, in healthy outpatients treated with a low *weekly* dose.
Critically ill inpatients on a high *daily* dose are much more likely to develop toxicity.
9/
Dr Carlos Chaccour wrote an excellent thread on Ivermectin a year ago👇
He points out that if ivermectin crosses the blood brain barrier it can interact with GABA receptors causing serious 🧠 side effects. This is more likely in inflamed patients on high dose ivermectin:
10/
He points out that if ivermectin crosses the blood brain barrier it can interact with GABA receptors causing serious 🧠 side effects. This is more likely in inflamed patients on high dose ivermectin:
10/
https://twitter.com/carlos_chaccour/status/1246432979485949959
Prior to COVID, there were case series describing serious toxicities from ivermectin. Most toxicities were neurological (& some were fatal).
These fatal events occurred at standard doses in previously healthy outpatients.
ncbi.nlm.nih.gov/pmc/articles/P…
11/
These fatal events occurred at standard doses in previously healthy outpatients.
ncbi.nlm.nih.gov/pmc/articles/P…
11/

The next time you hear that ivermectin is “perfectly safe” & “effective in COVID” remember:
- plasma or lung levels of ivermectin in vivo (Cmax) don’t get anywhere close to the IC50 required in vitro
- there ARE risks of potentially fatal neurological toxicity with ivermectin
- plasma or lung levels of ivermectin in vivo (Cmax) don’t get anywhere close to the IC50 required in vitro
- there ARE risks of potentially fatal neurological toxicity with ivermectin
• • •
Missing some Tweet in this thread? You can try to
force a refresh
































