First to note - is that there is no apparent association between GBS and #COVID19 #FOAMed #FOAMcc ucl.ac.uk/news/2020/dec/…
GBS is an ACUTE polyneuropathy (peripheral nervous system). Symmetrical in distribution. The onset is often over about 4 weeks and recovery often begins 2 weeks after progression has completed.
https://twitter.com/ManualOMedicine/status/1142477680006324225?s=20
There are 0.6-4 cases per 100,000 people across the world - fairly uniformly (annalsofian.org/article.asp?is…)
It can be a VERY serious disease. With the near-eradication of polio, GBS has become the most common cause of acute flaccid paralysis in developed countries. This has obvious implications in the ICU. 1/4 of patients will require IPPV. 3-11% will die of GBS complications.
To be specific, it's a heterogeneous disorder that involves the classical DEMYELINATING type of inflammatory polyradiculoneuropathy (AIDP) + the more rapid and usually less benign motor-sensory axonal forms (AMAN, AMSAN) and the anti-GQ1b spectrum of Miller-Fisher syndrome (MFS)
MFS is a more rare variant of GBS and usually presents with at least 2 of the following features: ataxia, areflexia, and ophthalmoplegia. MFS is commonly associated with the involvement of the lower cranial and facial nerves and does not usually involve motor weakness of limbs.
MFS variants including weakness of the respiratory system and limbs have been described. Another variant of MFS is Bickerstaff brainstem encephalitis (BBE) and involves altered consciousness, ataxia, ophthalmoparesis, and paradoxical hyperreflexia. ncbi.nlm.nih.gov/books/NBK50771…
GBS-like disease has been described in other medical conditions associated with acquired immunodeficiencies, transplantations, lymphomas, and biological treatments.
If we consider meningitis - we know the morphology of the 'typical' samples - but in GBS, it is the protein count that interests us... as well as some other things 
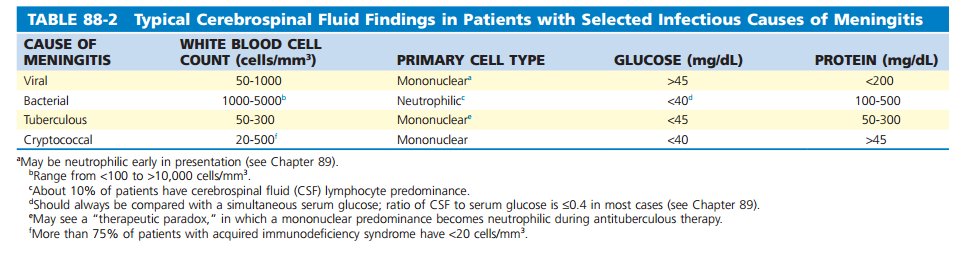
Albuminocytological dissociation (ACD), the classical alteration of the CSF in GBS was described in the original paper by Guillain, Barré and Strohl. This is an increased total protein concentration with normal total nucleated cell count.
ACD occurs in diseases that alter the blood-brain barrier, increase the production of protein or obstruct the flow of CSF.
During acute GBS, characteristic findings on CSF analysis include ACD = CSF protein (>0.55 g/L) without an elevation in white blood cells. The increase in CSF protein is thought to reflect the widespread inflammation of the nerve roots + incr BBB permeability.
CSF should be acellular. Protein levels may be normal during the 1st week of the illness, but the majority will have an ^protein if measured 2 or 3 weeks later. Incr CSF protein concentration in GBS has been mainly associated with increased permeability of the blood-CSF barrier.
This excellent flow diagram characterises the complex processes that contribute to GBS - including causes and therefore, things to test for... link.springer.com/chapter/10.100… 
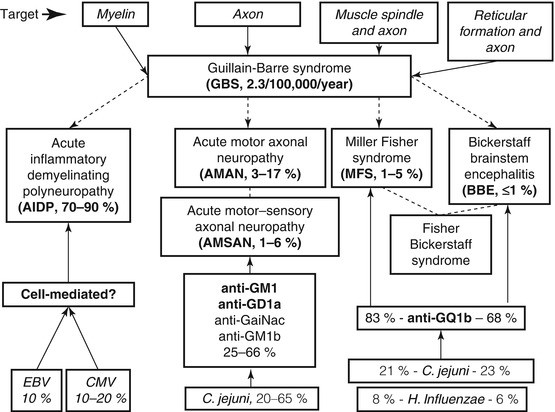
BIG exclusions of cause would be: Campylobacter jejuni enteritis (25-50% - so ask about BBQs!), Viral (CMV, EBV, Hepatitises, HIV, Flu, Zika, Chikungunya), Mycoplasma and VACCINATIONS such as flu/rabies.
Campylobacter jejuni (CJ) infections do = 25-50% of causes, but only <1% of those infected with CJ develop GBS symptoms. It causes auto-antibodies resulting from molecular mimicry (e.g. glycans expressed on bacterial lipooligosaccharides (LOS))
So.... GBS affects peripheral nerves, primarily spinal and cranial nerve roots. Autonomic nerves sometimes affected - so look for autonomic signs - BP/HR etc. 

TWO immune-injury pathologies at play:
1. Myelin sheath and related Schwann-cell components are targeted in acute inflammatory demyelinating polyneuropathy.
2. Membranes on the nerve axon are targeted in acute motor axonal neuropathy
1. Myelin sheath and related Schwann-cell components are targeted in acute inflammatory demyelinating polyneuropathy.
2. Membranes on the nerve axon are targeted in acute motor axonal neuropathy
GBS is mainly a humoral, rather than T-cell-mediated disorder, at least in the progressive phase of nerve injury. Recovery involves the dampening of the immune response and endogenous repair of nerves. litfl.com/guillain-barre…
The MECHANISM of cause affects the clinical phenotype and prognosis: CJ infections are usually associated with a pure motor axonal form of GBS, more severe limb weakness, and a serological antibody response directed against GM1 and GD1a gangliosides
Plasma Exchange (PLEX) was first shown in 1985 to be effective (non-selective removal of immunoglobulins, complement, and cytokines. pubmed.ncbi.nlm.nih.gov/4022342/ - confirmed in a 2012 Cochrane Review: pubmed.ncbi.nlm.nih.gov/22786475/ (Pic: pn.bmj.com/content/20/2/92) 
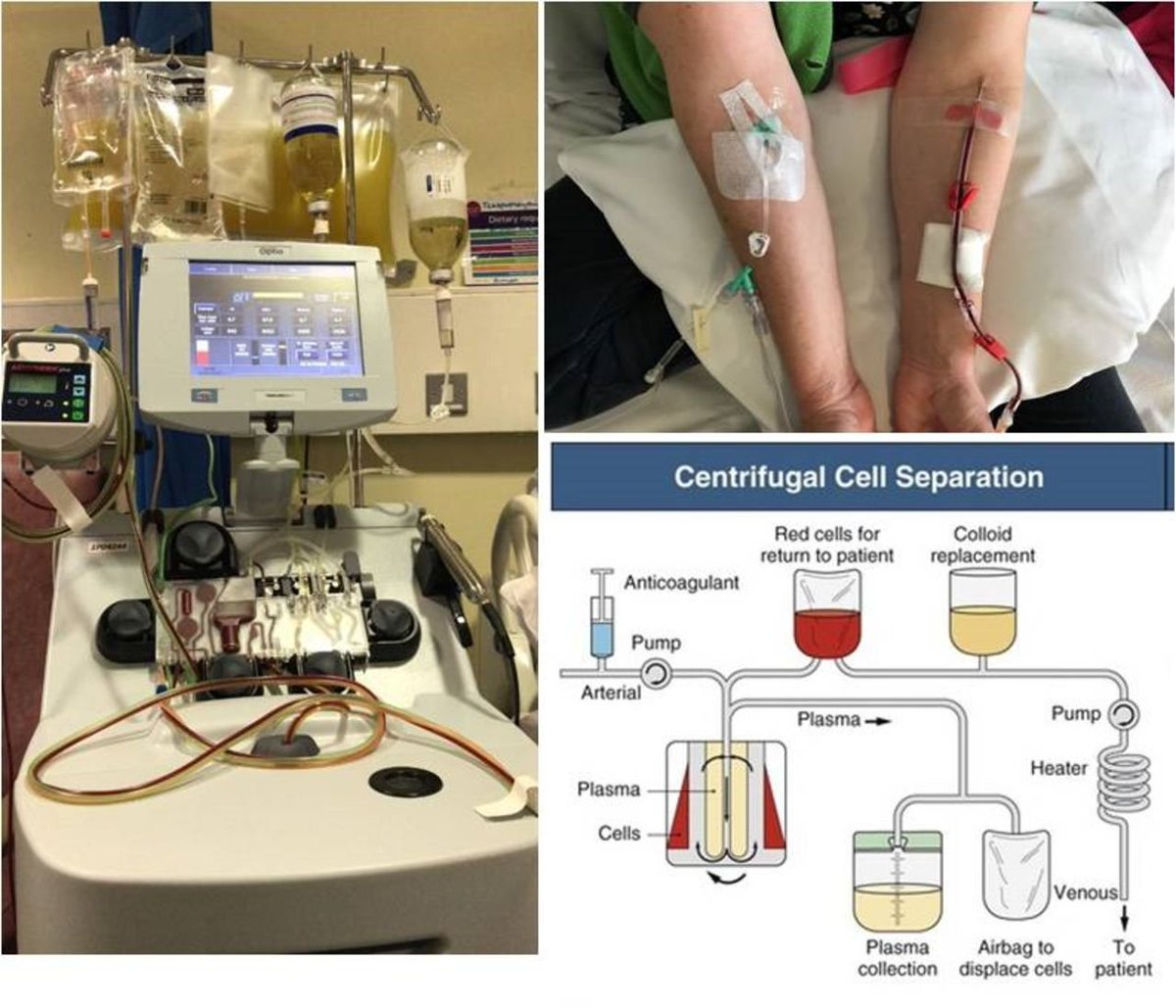
For severe GBS, the relative risk of improving one or more functional grades by 4 weeks after PE treatments was 1.64 (95% CI 1.37 to 1.96). Treatment also significantly reduced the number of patients requiring mechanical ventilation, shortened the time to extubation.
PLEX increased the number of patients achieving full strength at 1 year, and reduced the number of patients experiencing severe sequelae at 1 year.
These studies also demonstrated that treatment within 7 days is the most effective and that patients with mild GBS (able to ambulate at the time of treatment) still benefit from PE. pubmed.ncbi.nlm.nih.gov/9066350/
IV immunoglobulin is the other mainstay of treatment ncbi.nlm.nih.gov/pmc/articles/P… But it should be noted it is not without complications. Consider thrombotic risk in your patient, particularly in the COVID-19 era: pubmed.ncbi.nlm.nih.gov/16965420/ 

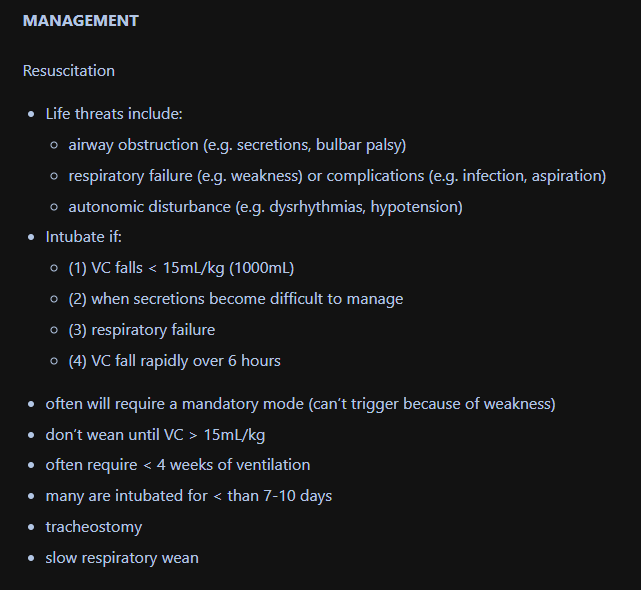
ICU considerations include intubation when the patient experiences muscular respiratory failure. Remember they will require full ventilation due to lack of triggering breaths. It is unlikely that a quick-wean will occur - so have a slow approach. litfl.com/guillain-barre… 
ICU Considerations + General GBS in "10 Steps" - nature.com/articles/s4158… 

Steroids do not have a role in GBS: ncbi.nlm.nih.gov/pmc/articles/P… 

Sometimes the prodrome can be unclear - so consider multiple factors. Sometimes, the initial presentation is muscular or radicular PAIN (back pain) which in 1/3 of cases precedes the weakness. 

Consider other causes: aafp.org/afp/2013/0201/… 

There are some very rare and odd mimics of GBS: onlinelibrary.wiley.com/doi/epdf/10.10…
POST-ICU CARE is a MAJOR consideration. It requires meticulous rehab and specialist care. There is significant mortality after discharge from ICU. jnnp.bmj.com/content/85/10/… 

In the UK, the mortality rate in ICU is 7.7% but the in-hospital mortality rate after ICU step-down is 16.7%. pubmed.ncbi.nlm.nih.gov/17881005/
• • •
Missing some Tweet in this thread? You can try to
force a refresh