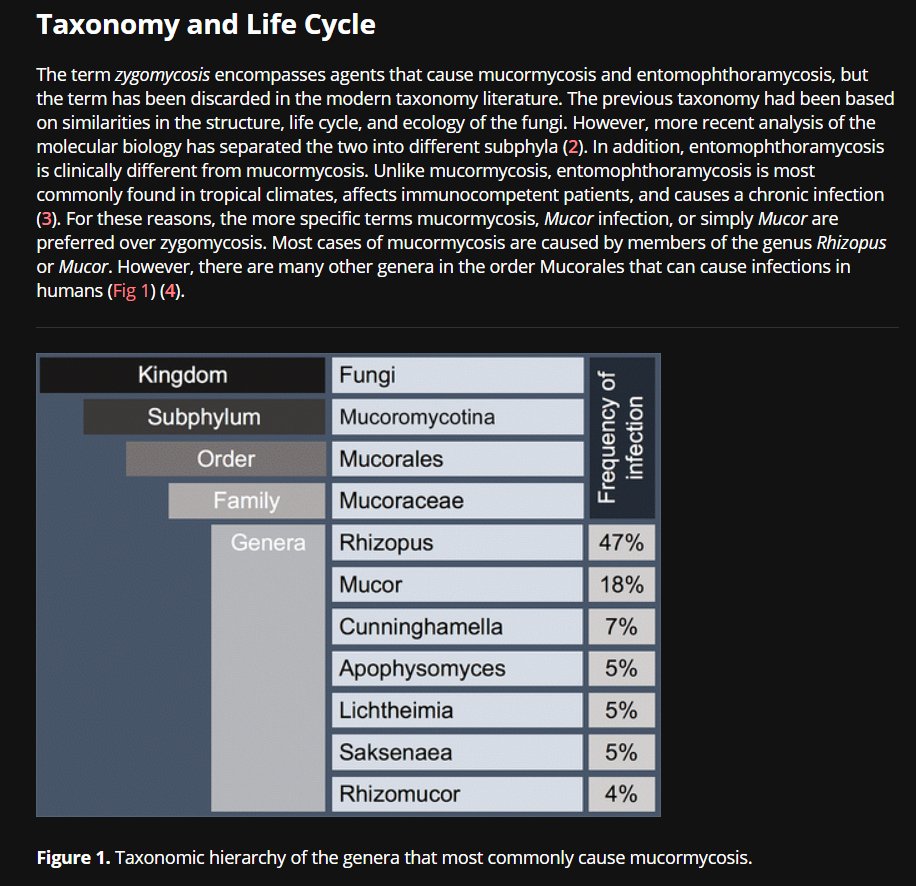
It's an invasive mould. Mucormycosis is a unifying term for infections belonging to 'Mucorales' - (so, Rhizopus, Mucor, Absidia etc). The fungi are filamentous. It's also all around us. pubs.rsna.org/doi/full/10.11… 
Pulmonary infection is clinically indistinguishable from more common moulds such as invasive pulmonary aspergillosis (IPA) - PLUS, it's not a reportable disease, which makes it (obviously) underreported.
Its prognosis is poor because of its high invasive power and its intrinsic low susceptibility to antifungal agents - they often just don't work.
Mucormycosis can affect: pulmonary, cutaneous (black lesions), GI and CNS as major loci of infection. Consider headache, facial pain, confusion, fever and sinusitis/purulent nasal discharge as suspicious.
When we consider invasive fungal infx in ICU, we think of the immunocompromised - so actually we should consider a whole host of organisms... link.springer.com/article/10.100… 
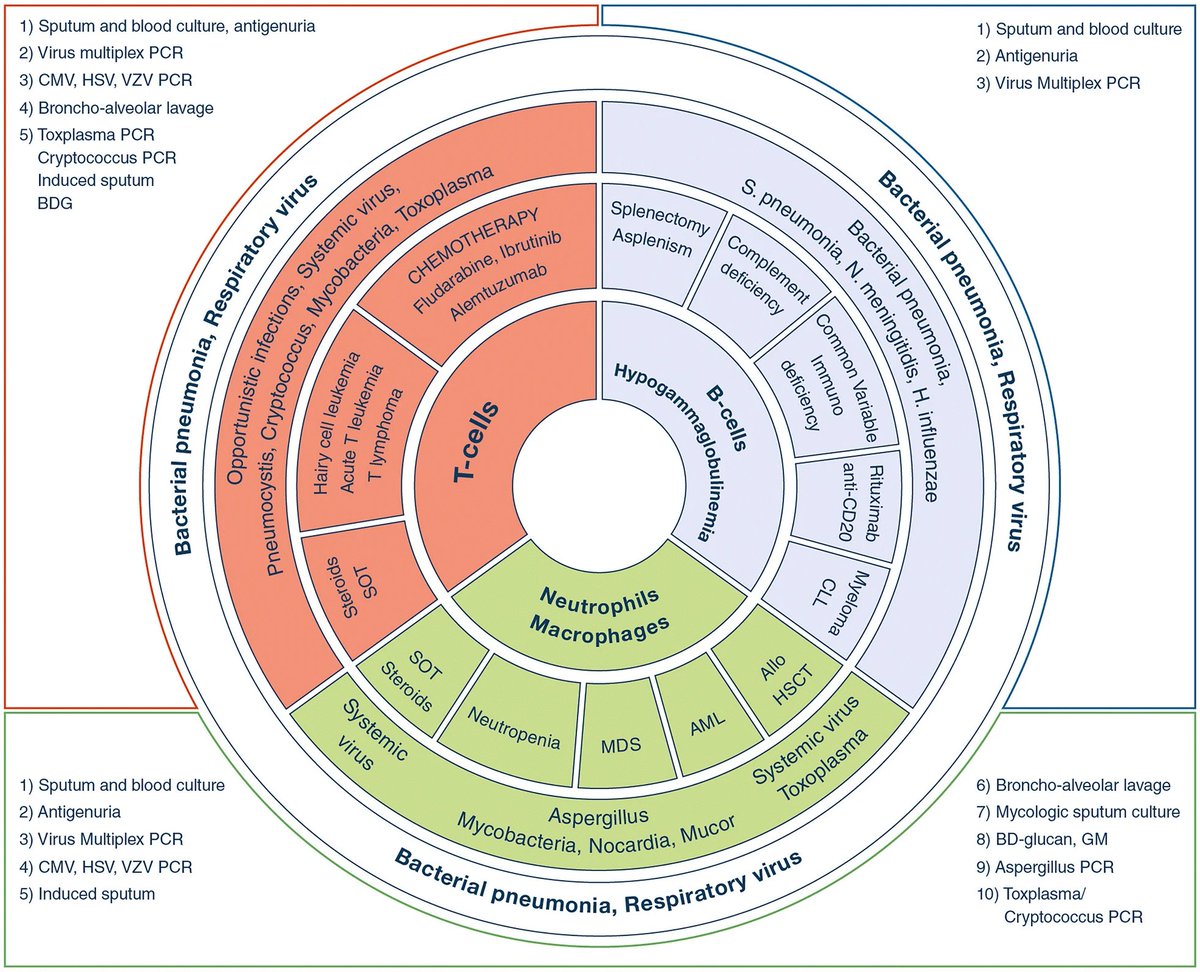
We also worry about the lungs link.springer.com/article/10.100… 

In fact, pneumonia in the immunocompromised patient is a rather large area, as demonstrated by @LITFLblog here: litfl.com/wp-content/upl… 

So why the focus on Mucormycosis at the moment? Well - it's been thrown into the spotlight in India during #COVID19 - bbc.com/future/article… 

There has always been a link with mucormycosis and DIABETES (academic.oup.com/mmy/article/56…) - of which the incidence is high in India (77 million) (2nd in world after China) thehindu.com/sci-tech/healt…
A recent summary of #COVID19-associated mucormycosis showed 94% of patients had diabetes mdpi.com/2309-608X/7/4/…
Before the pandemic, mucormycosis was already far more common in India than in any other country. It affects an estimated 14 in every 100,000 people in India compared to 0.06 per 100,000 in Australia, for example. ncbi.nlm.nih.gov/pmc/articles/P…
Mucormycosis is often associated more with its profound action against soft-tissue and cutaneous layers - it was once called ZYGOmycosis. Rhino-orbito-cerebral mucormycosis has striking clinical pictures associated with it: thelancet.com/journals/lanin… 

The scope of the problem is laid bare in the figures surrounding its mortality. Even though it is usually a rare fungal infection - it has a 40-80% mortality - and when there is CNS involvement, this is >80% thelancet.com/journals/lanin…
In general, the most at-risk groups are haematology patients who have had a haematopoietic stem cell transplantation (HSCT).
So - suspected OR confirmed mucormycosis is an emergency - and there are guidelines of what to consider. RAPID action is a priority: thelancet.com/journals/lanin… 

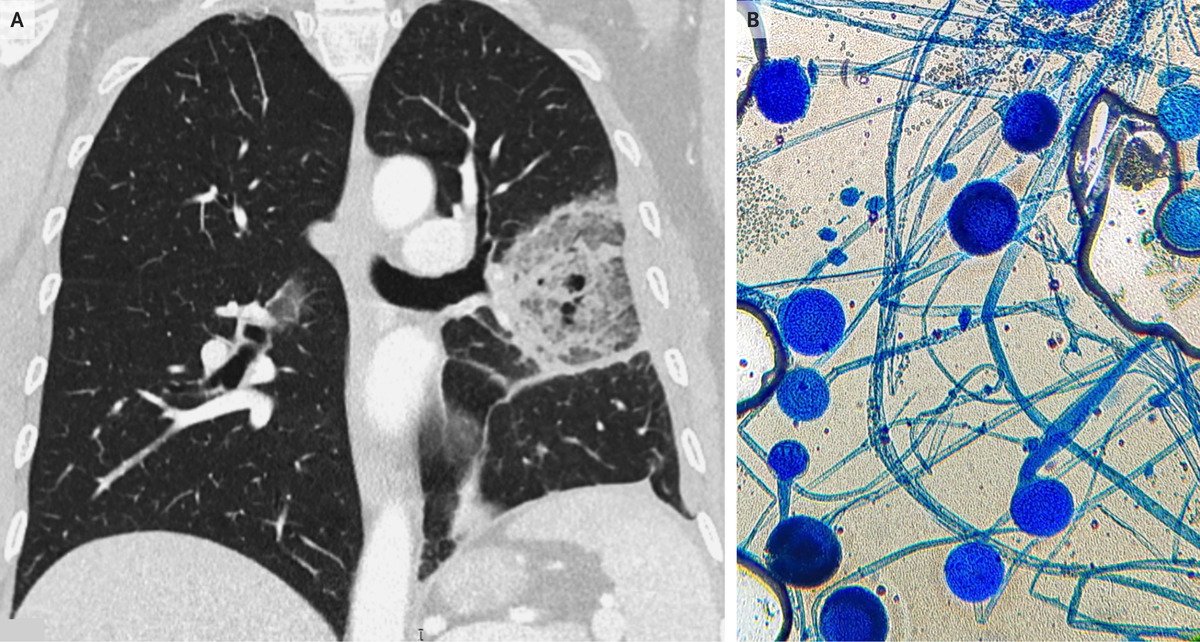
Focusing on PULMONARY: One can sometimes appreciate a 'REVERSE HALO' sign - an area of ground-glass opacity surrounded by a ring of consolidation on thoracic CT, or vessel occlusion on CTPA. thelancet.com/journals/lanin… 

There are really high detail images of case presentations of pulmonary mucormycosis on @Radiopaedia here: radiopaedia.org/articles/pulmo… (Case courtesy of Dr David Holcdorf, Radiopaedia.org, rID: 64718) 

In diabetic pts with facial pain, sinusitis, proptosis, ophthalmoplegia, or newly diagnosed amaurosis, or both --> cranial CT or MRI to look for sinusitis. If sinusitis is diagnosed, endoscopy is strongly recommended to diagnose. Biopsy. MRI preferred.
As mentioned before - CNS involvement is associated with a very poor prognosis (>80%)
Of interest histopathologically, is that the morphology of mucormycosis can be confused with aspergillus - which is more common: 

The mainstay of treatment is debridement of areas amenable to surgery and aggressive antifungal drugs thelancet.com/journals/lanin… 




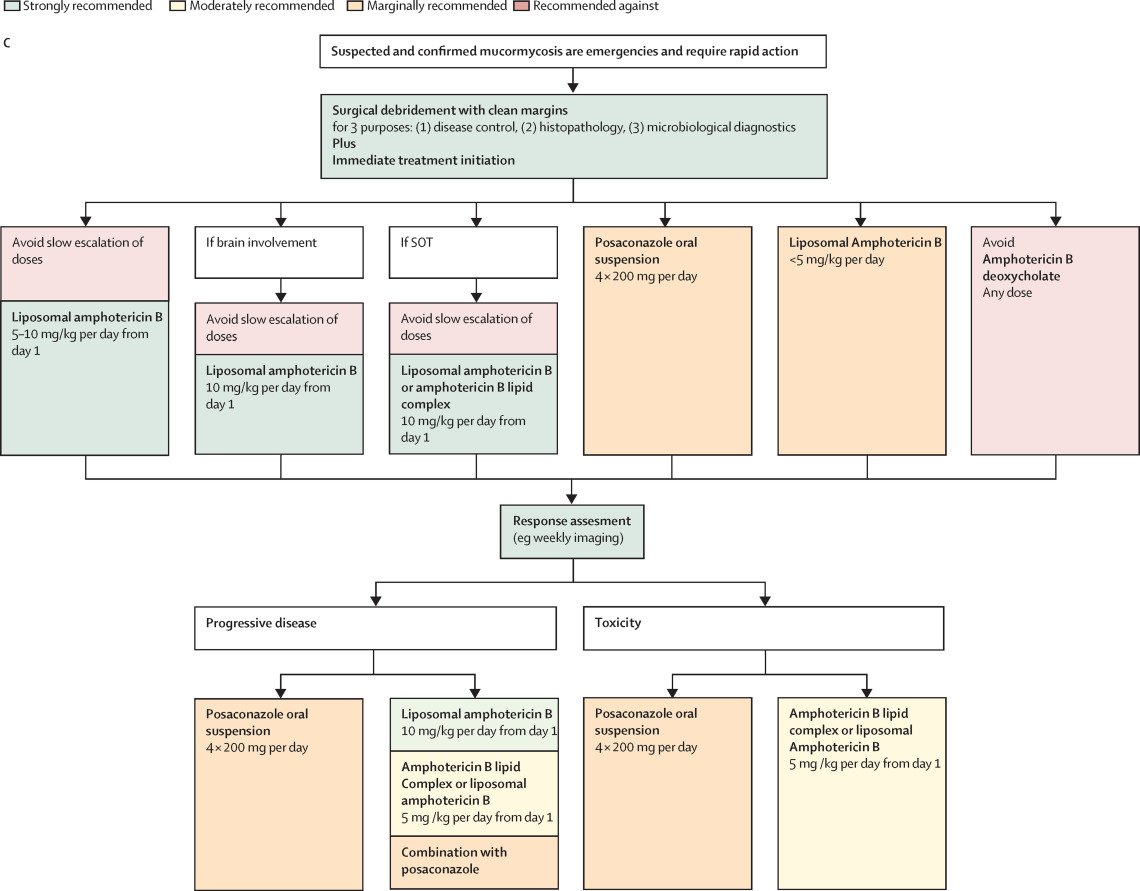
A full range of treatment discussions and rationale is available here: thelancet.com/cms/10.1016/S1…
If amenable to surgery - and cutaneous - treatment is long and typically over 4-6 weeks of repeated surgery along with aggressive antifungal drugs. magonlinelibrary.com/doi/full/10.12…
One of the drugs, amphotericin (used for >60 years) is associated with nephrotoxicity, which is a large consideration in ICU. A great article/summary is here: link.springer.com/article/10.100…
In terms of rarer considerations, mycosis can simultaneously cause both invasive infection and a host allergic reaction: bmcpulmmed.biomedcentral.com/articles/10.11… 

Whilst diagnosis is often clinical and radiological - samples should be taken - sputum, secretions, biopsies and BAL - academic.oup.com/cid/article/54… 

An interesting and modern discussion of a #COVID19 patient in ICU with pulmonary mucormycosis: link.springer.com/article/10.100… This case highlights how this #COVID19 might impair the immune response, exposing patients to developing opportunistic infections and leading to worse outcomes. 

Have a look at all of Propofology's Twitter output for conferences and Tweetorials over the years: linktr.ee/propofology All in one place for ease of navigation! #FOAMed #FOAMcc
Other excellent resources on fungal infections in the ICU are: accp.com/docs/bookstore… and academic.oup.com/bjaed/article/… 


• • •
Missing some Tweet in this thread? You can try to
force a refresh