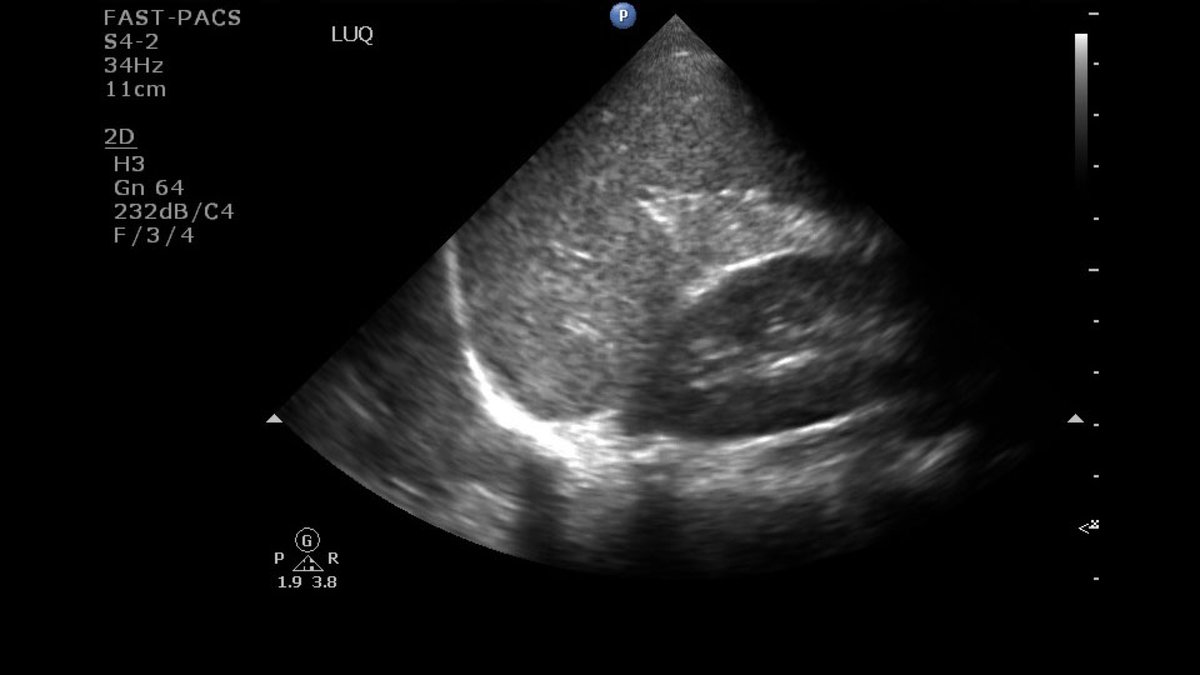
Patient with epig pain and multiple ED visits with neg CT and non-specific labs - but persistent pain. What do you do? GI cocktail + famotidine and discharge? How about a little #POCUS first. #FOAMed #FOAMus #Ultrasound #MedTwitter @mtabbut @laurarbrownmd @RJonesSonoEM
And the transverse view. What do you think now? Poll below in thread. #Whatsthedx #EmergencyMedicine @DianeGramer @SLWerner_EM @ClaridgeJeffrey @vanessapho @ladha_prerna
What do you think?
Patient with acute cholecystitis. Note here the stones layering in the dependent portion of the gallbladder (red arrows) with the posterior dark shadowing dark shadowing (blue arrows) 



Take home points:
1. Don't forget to consider the gallbladder in patients with epig pain and non-specific labs.
2. Cholecystitis is a clinical dx with sono findings (stones + wall thick, biliary dissension, PCF, sono-murphy sign).
1. Don't forget to consider the gallbladder in patients with epig pain and non-specific labs.
2. Cholecystitis is a clinical dx with sono findings (stones + wall thick, biliary dissension, PCF, sono-murphy sign).
Take home points 2/2:
3. If pt condition changes or doesn't improve - don't be afraid to re-image - perhaps a different way.
Good article about #POCUS for Acute Chole. pubmed.ncbi.nlm.nih.gov/20138397/
3. If pt condition changes or doesn't improve - don't be afraid to re-image - perhaps a different way.
Good article about #POCUS for Acute Chole. pubmed.ncbi.nlm.nih.gov/20138397/
• • •
Missing some Tweet in this thread? You can try to
force a refresh