The CDC guidelines for #LongCOVID are out!!!
@itsbodypolitic and @patientled worked together to give feedback on these and it's really emotional to see our research, including the first report we did back in April 2020, cited here. 1/
cdc.gov/coronavirus/20…
@itsbodypolitic and @patientled worked together to give feedback on these and it's really emotional to see our research, including the first report we did back in April 2020, cited here. 1/
cdc.gov/coronavirus/20…
It's going to take a while to go through & see what ended up in here, but a few things stand out to me that we pushed hard for:
A) The inclusion of a comprehensive symptom list, including PEM (and a definition for PEM!) and lesser-discussed but common symptoms. 2/
A) The inclusion of a comprehensive symptom list, including PEM (and a definition for PEM!) and lesser-discussed but common symptoms. 2/

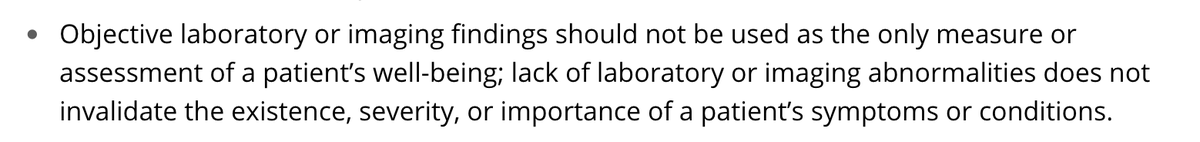
B) Instructions not to use lab confirmation: "Objective laboratory/imaging findings shouldn't be used as the only assessment of a patient’s well-being; lack of laboratory/imaging abnormalities does not invalidate the existence, severity, or importance of a patient’s symptoms." 3/ 


C) A warning against the increased use of psychologizing #LongCOVID patients. Essentially a request to medical providers to learn about stigma and to be empathetic! 4/ 

D) An acknowledgment about common overlapping conditions and diagnoses including dysautonomia, ME, and MCAS, and acknowledgments that people with post-exertional malaise may benefit from pacing, & also explicit instructions to be careful with exercise testing in PEM patients. 5/ 



E) Less of a focus on physical rehabilitation, and equal inclusion of occupational therapy, speech and language therapy, and neurological rehabilitation. 6/ 

• • •
Missing some Tweet in this thread? You can try to
force a refresh