Covid (@UCSF) Chronicles, Day 495
When I began my tweets 494d ago, it was before we had reliable local, US, or world data. So I focused on data from @UCSFHospitals. Today, we’re awash in data, yet I find my hospital's data still provides a unique lens into our situation. (1/20)
When I began my tweets 494d ago, it was before we had reliable local, US, or world data. So I focused on data from @UCSFHospitals. Today, we’re awash in data, yet I find my hospital's data still provides a unique lens into our situation. (1/20)
So today, a few data points from @UCSF, with my interpretation. They reinforce the case that the combo of Delta & relaxed behavior is leading to a powerful & worrisome upsurge that requires a change in approach. I knew things were bad, but it’s even worse than I thought. (2/20)
What’s particularly noteworthy about @UCSF experience is that it’s in a city w/ the nation’s highest vax rate. And cases are rising fast in our employees, of whom 93% are vaxxed. (Special thanks to Ralph Gonzales, Bob Kosnik & @SaraMurrayMD for some of the data.) Here goes:(3/20)
Let’s start w/ context: in SF, 69% of all people (76% >age 12) are fully vaccinated. (Vs CA, 52% of population; U.S. 50%.) So the surge in SF is especially sobering, since it indicates that we’ll need an immunity rate far higher than 70-75% to achieve “local” herd immunity.(4/20)
Let's look at hospitalizations. On June 1, we had one Covid patient in our ~700-bed @UCSFHospitals (we never quite got to zero); none were in the ICU.
Today we have 28 hospitalized pts @UCSFHospitals: 15 on the floor & 13 in the ICU (7 on vents). A staggering increase. (5/20)
Today we have 28 hospitalized pts @UCSFHospitals: 15 on the floor & 13 in the ICU (7 on vents). A staggering increase. (5/20)

I don’t have the vaccinated/unvaxxed breakdown for today's census, but it’s been running >90% unvaxxed in recent wks. When we do see vaccinated patients in the hospital, many are immunocompromised (a group in which vaccine’s effect is attenuated – we need a new approach). (6/20)
My interpretation: even in a city with very high vaccination levels, serious cases have skyrocketed, mostly in unvaccinated people. Now think about what will happen in a region in which 60-70% of the population is unvaccinated, not SF’s 25-30%. Really scary stuff. (7/20)
In April, I wrote @washingtonpost that “this is the most dangerous moment to be unvaccinated.” washingtonpost.com/opinions/2021/….
I was wrong – now is even MORE dangerous since Delta has taken over, caution's been thrown to the wind, and there’s far more virus around. (8/20)
I was wrong – now is even MORE dangerous since Delta has taken over, caution's been thrown to the wind, and there’s far more virus around. (8/20)
How much virus is around? Since early in the pandemic, I’ve used a piece of data available @UCSF (not publicly) to estimate the chances that a person who feels well in SF is carrying the virus. It’s our “asymptomatic test positivity rate” and it comes from the fact … (9/20)
… that we test all our hospitalized & ED patients who have no Covid symptoms, as well as people undergoing surgeries or procedures like cardiac caths. That fraction was as low as about 0.1% in early June – which was pretty reassuring – it meant that the chances that…(10/20)
… a person near you in a SF store had asymptomatic Covid was ~1-in-1000.
Today, it’s 2.14%! So now that asymptomatic person has a ~1-in-50 chance of being positive. (And this % may be an underestimate since our pts are older than avg, a group with a higher vax rate). (11/20)
Today, it’s 2.14%! So now that asymptomatic person has a ~1-in-50 chance of being positive. (And this % may be an underestimate since our pts are older than avg, a group with a higher vax rate). (11/20)
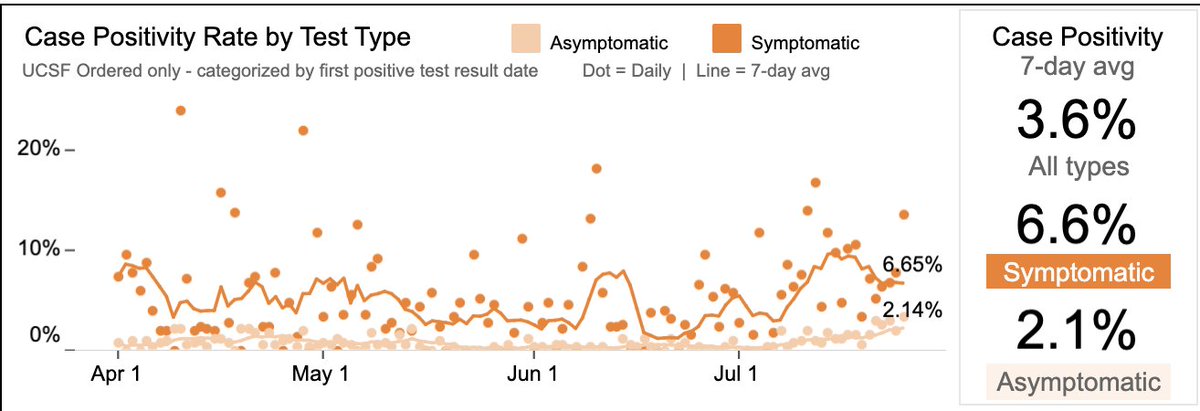
My interpretation: the risk of getting Covid is related to your vax status, whether you're taking steps to lower risk (masking, etc), & whether you’re exposed to the virus. Even in highly vaccinated SF, the odds of being exposed have gone up ~ 20-fold since June 1. (12/20)
The point's been made that, if everybody’s vaccinated, all infections will be in vaccinated people (even if vax efficacy stays high). Among @UCSF students/employees, we’re not at 100% but we’re close: 32,550 of our 35,018 people (93%) are vaccinated. (Mandate starts 9/1.) (13/20)
Given this vax rate, it shouldn’t surprise that 83% (77/93) of our July cases are in vaccinated folks. This DOESN’T mean vax isn't working – calculated efficacy from these data is 82%. We’d expect 422 cases in our vaccinated population, not 77, if the vaccine didn’t work. (14/20) 
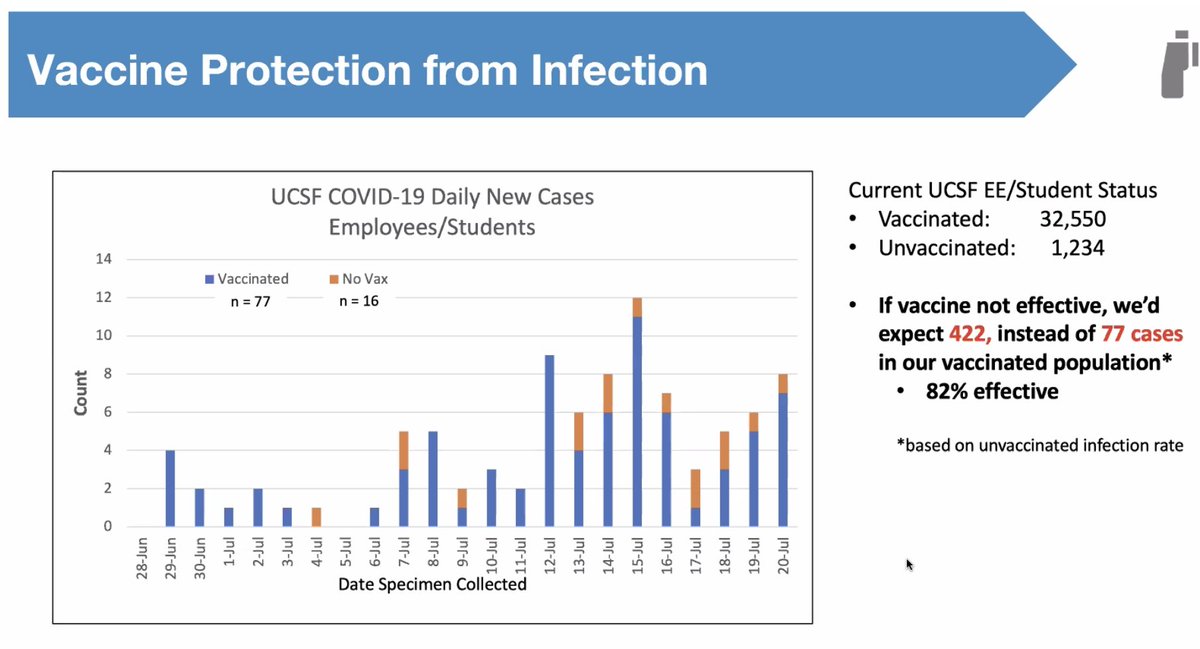
At least @UCSF, we see no evidence that efficacy is waning: no case uptick in those vaxxed in Dec-Jan vs. more recently. And the vaccines are still >90% effective in preventing severe illness: only 1 these 77 breakthrough infections required a (brief) hospitalization. (15/20)
(This always raises the question of why I, as a vaccinated person, still don't want to get a breakthrough case of Covid. If you're interested, I answered that one here: sfgate.com/bayarea/articl… (16/20)
Taken together, it’s clear that – even in highly vaccinated SF; it's also a city in which people remained pretty careful despite relaxed rules – we're experiencing a unmistakable surge. The vaccines work great, but, as we now appreciate, they don’t prevent all infections. (17/20)
Even w/ surge, we’re not overwhelmed @UCSF, thanks to vaccines. Scary to consider regions where vulnerable % is much higher. I’m glad the U.S. is finally seeing an uptick in vaccination, but it won’t help for a month (since vax efficacy of dose 1 against Delta is so low).(18/20)
As @DrLeanaWen convincingly argued @washingtonpost, it's time to add back restrictions, esp. indoor masking. washingtonpost.com/opinions/2021/…
As for me, it’s back to double-masks indoors & N95s on planes. And sadly, that’s it for indoor dining for a while. None of this pleases me.(19/20)
As for me, it’s back to double-masks indoors & N95s on planes. And sadly, that’s it for indoor dining for a while. None of this pleases me.(19/20)
Along with renewed restrictions, it’s clear that gentle persuasion did not achieve the vax rate we need to defeat Covid. Yes, the politics are hard, but dying is worse, as is re-tanking the economy. It’s time for vaccine mandates – nothing else gets us where we need to go.(20/20)
• • •
Missing some Tweet in this thread? You can try to
force a refresh






