1/ AIRBORNE TRANSMISSION OF RESPIRATORY VIRUSES
A new peer-reviewed paper in @ScienceMagazine, reviewing the scientific literature on this topic. We conclude it is important not just for COVID-19, but also for other respiratory diseases such as the flu
science.sciencemag.org/content/373/65…
A new peer-reviewed paper in @ScienceMagazine, reviewing the scientific literature on this topic. We conclude it is important not just for COVID-19, but also for other respiratory diseases such as the flu
science.sciencemag.org/content/373/65…
2/ An honor to have worked in a multidisciplinary team across virology, pulmonary physiology, aerosol science, and sociology with Chia Wang, @kprather88, @Lakdawala_Lab, Josué Sznitman, @linseymarr, and @zeynep
Will try to summarize the paper and give some context in this thread
Will try to summarize the paper and give some context in this thread
3/ Brief intro: what are droplet vs. airborne transmission?
"Droplets" are larger balls of saliva and respiratory fluid, that we emit when we talk, shout, sing, cough or sneeze.
They behave like projectiles, and fall to the ground within 1-2 m of the infected person
"Droplets" are larger balls of saliva and respiratory fluid, that we emit when we talk, shout, sing, cough or sneeze.
They behave like projectiles, and fall to the ground within 1-2 m of the infected person

4/ Droplets infect by impacting on the eyes, nostrils, or mouth.
Basic physics shows that droplets are larger than 100 microns (1 micron = 1 millionth of a meter):
onlinelibrary.wiley.com/doi/10.1111/j.….
(Image adapted from @Don_Milton academic.oup.com/jpids/article/…)
Basic physics shows that droplets are larger than 100 microns (1 micron = 1 millionth of a meter):
onlinelibrary.wiley.com/doi/10.1111/j.….
(Image adapted from @Don_Milton academic.oup.com/jpids/article/…)

5/ Particles smaller than 100 microns float further than 1-2 m, stay suspended in the air, and can be inhaled.
These are aerosols.
Aerosols infect by *inhalation*, NOT by impact. We breathe them in.
These are aerosols.
Aerosols infect by *inhalation*, NOT by impact. We breathe them in.

6/ As an aside, we have known for a long time that transmission through surfaces is not important. There are zero proven cases for COVID-19, and it wouldn't be so hard to prove if it was important.
So it is really droplets vs. aerosols
nature.com/articles/d4158…
So it is really droplets vs. aerosols
nature.com/articles/d4158…
7/ The short version of new review in @ScienceMagazine (TL;DR -- too long, didn't read it):
- It is not just COVID-19, but all or almost all respiratory diseases likely have an important component of airborne transmission
- It is not just COVID-19, but all or almost all respiratory diseases likely have an important component of airborne transmission
8/ - The same historical and political reasons that slowed recognition of airborne trans. for COVID-19 for more than a year, also impacted other diseases (e.g. flu)
- Once you accept it is airborne, there are *many* effective things we can do to reduce the spread of a virus
- Once you accept it is airborne, there are *many* effective things we can do to reduce the spread of a virus
9/ This is a big change for public health.
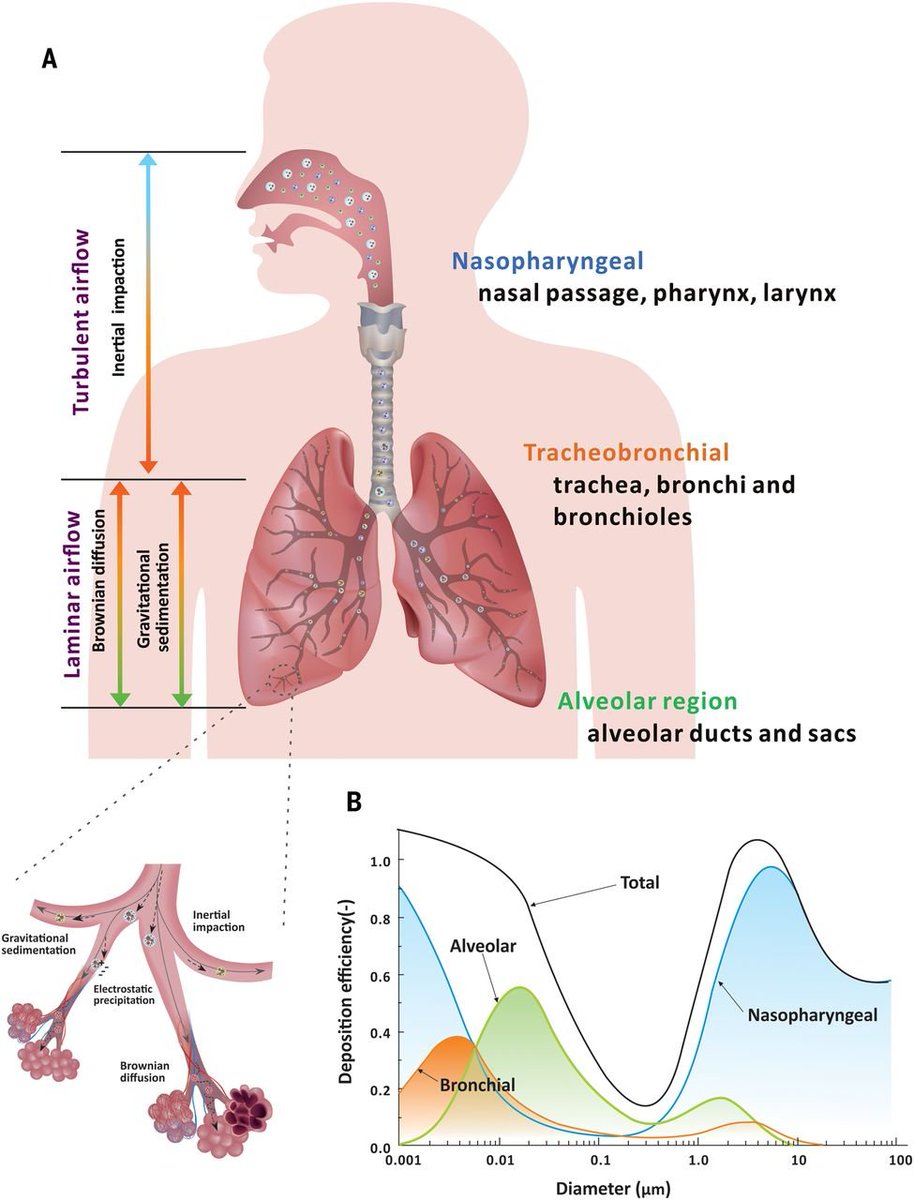
For example, despite extensive evidence supporting airborne transmission of the flu (that was available before the COVID-19 pandemic), @WHO describes it as a droplet / fomite disease:
For example, despite extensive evidence supporting airborne transmission of the flu (that was available before the COVID-19 pandemic), @WHO describes it as a droplet / fomite disease:

10/ The same is true for @CDCgov.
BTW the text is almost identical to what the CDC erroneously told us for many months about how COVID-19 spread. (They still explain it quite confusingly, as we will discuss)
cdc.gov/flu/about/dise…
BTW the text is almost identical to what the CDC erroneously told us for many months about how COVID-19 spread. (They still explain it quite confusingly, as we will discuss)
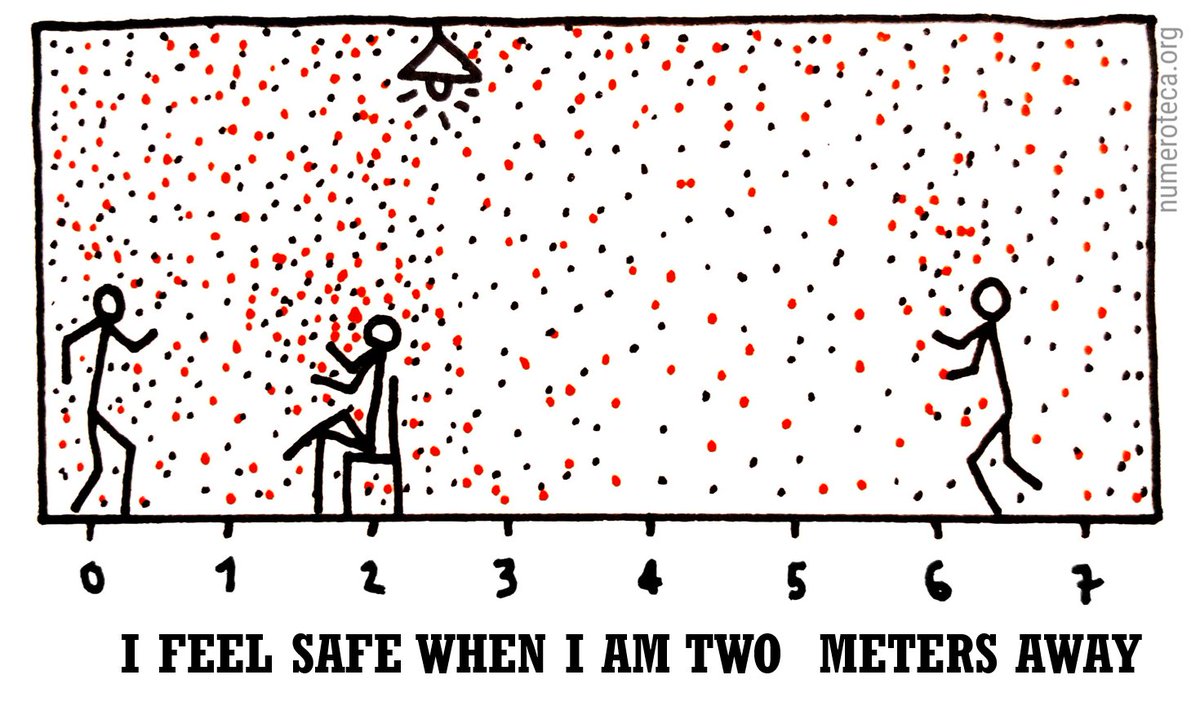
cdc.gov/flu/about/dise…

11/ There has been a lot of confusion, with droplets described by some as "magical droplets" which:
- Fall near the infected person
- Somehow they can infect by inhalation
- In poorly ventilated locations, somehow they float
This is not consistent with physics.
A visual:
- Fall near the infected person
- Somehow they can infect by inhalation
- In poorly ventilated locations, somehow they float
This is not consistent with physics.
A visual:
12/ As we summarize in the review & previous literature, that's not possible
If they fall within 1-2 m of person, they behave like projectiles & are > 100 um (> 300 um when talking)
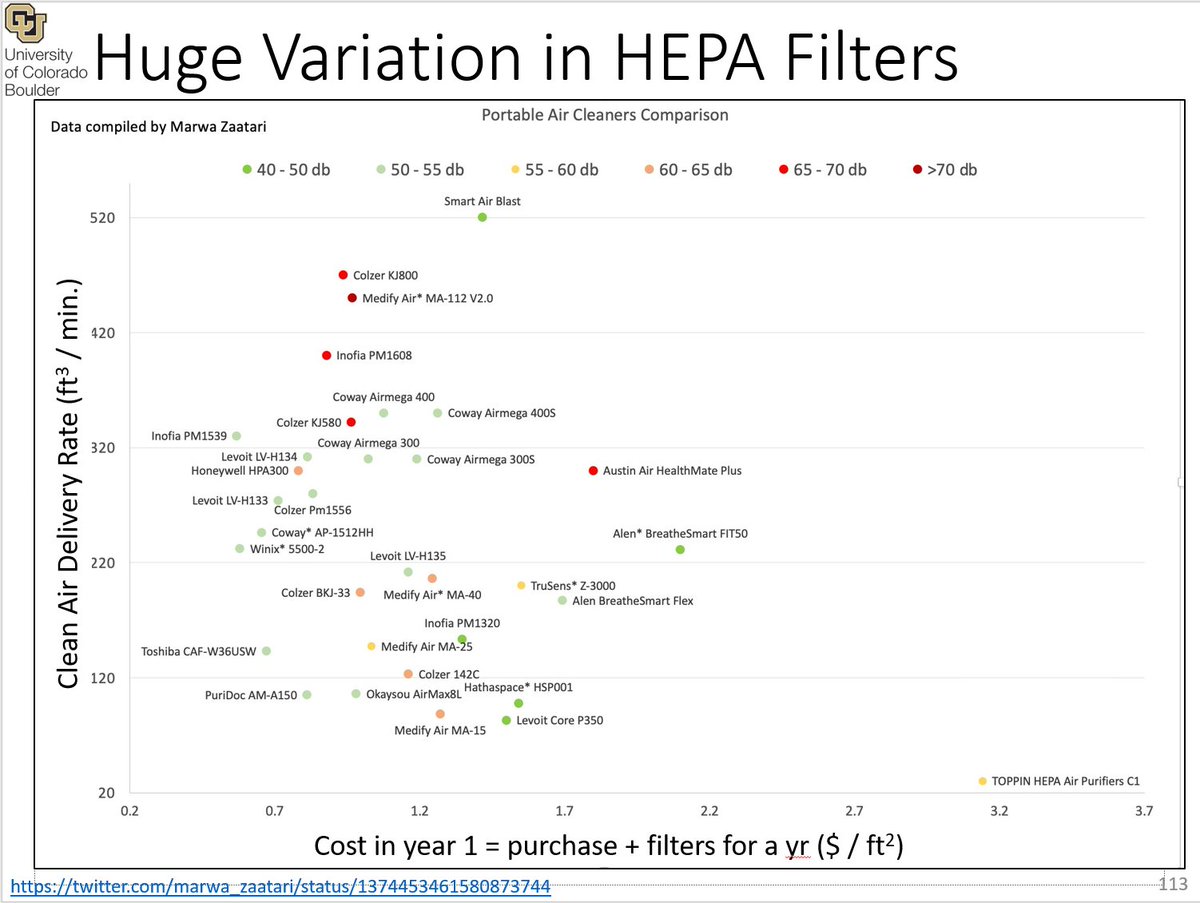
If they can infect in poorly ventilated room, they are aerosols, < 100 um, infect by inhalation
If they fall within 1-2 m of person, they behave like projectiles & are > 100 um (> 300 um when talking)
If they can infect in poorly ventilated room, they are aerosols, < 100 um, infect by inhalation

13/ A previous tweetorial on this issue of the size limiting droplets (projectiles like "angry birds") from aerosols ("inhaled like smoke") is here:
https://twitter.com/jljcolorado/status/1292880342227984385
14/ In the new review paper in @ScienceMagazine we reviewed multiple types of evidence from the scientific literature about multiple viruses, which are summarized in this table. 

15/ We investigated SARS-CoV, SARS-CoV-2, MERS-CoV, influenza virus, rhinovirus, measles virus, and RSV
There is evidence for airborne transmission for additional viruses, but we chose to focus on those given their importance & the limited length available for the review
There is evidence for airborne transmission for additional viruses, but we chose to focus on those given their importance & the limited length available for the review

16/ Types of evidence investigated include virus detection in indoor air samples (PCR or cell culture), demonstration of airborne transmission in animal models, laboratory / clinical studies, epidemiological analyses, simulation & modeling, and aerosol size-resolved measurements
17/ All types of evidence support the importance of airborne transmission for SARS-CoV-2 and influenza virus, and many types of evidence are also available for the other diseases 

18/ Historically, airborne transmission was considered unproven for ANY disease in 1910-1962. All resp. diseases are considered droplet / fomite
1962 tuberculosis (bacterium) is accepted as airborne based on animal models
1980 measles & chickenpox accepted from epi analyses
1962 tuberculosis (bacterium) is accepted as airborne based on animal models
1980 measles & chickenpox accepted from epi analyses
19/ The attitude over the last century has been that a respiratory disease is transmitted by droplets, unless there is undeniable evidence to the contrary.
Played out for COVID-19, and also for flu and other diseases.
More details here (now in press): papers.ssrn.com/sol3/papers.cf…
Played out for COVID-19, and also for flu and other diseases.
More details here (now in press): papers.ssrn.com/sol3/papers.cf…
19/ E.g. we have been told over the last year "if COVID was airborne like measles, we could tell immediately"
Except... measles was described for 70 years as droplet / fomite, until 1980s, accepted bc obvious superspreading & long distance transmission
pediatrics.aappublications.org/content/75/4/6…
Except... measles was described for 70 years as droplet / fomite, until 1980s, accepted bc obvious superspreading & long distance transmission
pediatrics.aappublications.org/content/75/4/6…

20/ But it turns out that for the flu we had lots of evidence of all types (before the COVID-19 pandemic) that it was airborne.
E.g. superspreading events:
pubmed.ncbi.nlm.nih.gov/463858/
E.g. superspreading events:
pubmed.ncbi.nlm.nih.gov/463858/
21/ And infectious flu virus has been sampled from the breath of infected people:
pnas.org/content/115/5/…
pnas.org/content/115/5/…
22/ And infectious flu virus has been found in room air:
journals.asm.org/doi/10.1128/ms…
(Something that has *never* been achieved for the well-accepted airborne diseases, tuberculosis, measles, or chickenpox)
journals.asm.org/doi/10.1128/ms…
(Something that has *never* been achieved for the well-accepted airborne diseases, tuberculosis, measles, or chickenpox)
23/ And airborne transmission of the flu has been demonstrated with animal models (e.g. ferrets):
www-proquest-com.colorado.idm.oclc.org/docview/200966…
www-proquest-com.colorado.idm.oclc.org/docview/200966…
24/ And epidemiological analysis conclude that aerosol (=airborne) transmission is important for the flu:
nature.com/articles/ncomm…
nature.com/articles/ncomm…
25/ And influenza virus stays infectious in the air for 1 hour or more, so it can be inhaled:
academic.oup.com/jid/article/21…
academic.oup.com/jid/article/21…
26/ And influenza virus (and other pathogens, including SARS-CoV-2) are more concentrated in smaller aerosols:
thelancet.com/journals/lanre…
thelancet.com/journals/lanre…
26/ And influenza displays "anisotropic infection", i.e. infection by inhalation of small aerosols requires a lower dose and leads to a more serious infection than deposition of droplets in the nose:
(also for COVID in animals)
doi.org/10.3181/003797…
doi.org/10.1002/jmv.18…
(also for COVID in animals)
doi.org/10.3181/003797…
doi.org/10.1002/jmv.18…
27/ In summary, there is a ton of evidence of many types supporting airborne transmission of the flu. But like for COVID-19, it has been ignored for decades because it contradicted the established droplet dogma.
28/ We also review the evidence for COVID-19 in the @ScienceMagazine review, but a perhaps easier paper to read is this one on @TheLancet:
https://twitter.com/jljcolorado/status/1383566908797059078
29/ There are many more details, but I'll switch to the other 2 topics we cover (detailed mechanism of airborne transmission, and how to reduce it) in the interest of "brevity"
(I know, I know a 50 tweet thread is not brief, what can I do!)
(I know, I know a 50 tweet thread is not brief, what can I do!)
30/ So we review the detailed processes involved in airborne transmission, including:
- the generation and exhalation of aerosols
- the transport through the air
- the inhalation, deposition, and infection of a susceptible person
And the key factors impacting them
- the generation and exhalation of aerosols
- the transport through the air
- the inhalation, deposition, and infection of a susceptible person
And the key factors impacting them

31/ Generation and exhalation of infectious aerosols:
- Bronquiolar aerosols formed by shear forces that destabilize air/mucus interface
- Laryngeal aerosols formed through vocal fold vibrations (vocalization)
- Oral aerosols and droplets are formed from saliva
- Bronquiolar aerosols formed by shear forces that destabilize air/mucus interface
- Laryngeal aerosols formed through vocal fold vibrations (vocalization)
- Oral aerosols and droplets are formed from saliva

32/ Transport through the air: Once the aerosols are in the air, multiple processes are important.
- Initial size + drying determines whether they settle quickly (droplets), slowly (larger aerosols) or very slowly (smaller aerosols)
- Initial size + drying determines whether they settle quickly (droplets), slowly (larger aerosols) or very slowly (smaller aerosols)

33/ The physico-chemical properties of virus-containing aerosols matter a lot for virus inactivation vs. time ("virus survival")
E.g. the water content (which changes with relative humidity), temperature and pH.
Exact dependences vary for different viruses
E.g. the water content (which changes with relative humidity), temperature and pH.
Exact dependences vary for different viruses

34/ As we were discussing earlier, size is critical to understand how fast they settle.
To really settle in ~5 seconds, within ~1 m of the infected person, they need to be > 100 microns (um).
If they are 5 microns (that @WHO still calls "droplets") they settle in > 30 min
To really settle in ~5 seconds, within ~1 m of the infected person, they need to be > 100 microns (um).
If they are 5 microns (that @WHO still calls "droplets") they settle in > 30 min

35/ For decades, @CDCgov, @WHO and the medical literature have erroneously stated that the aerosol-droplet boundary is at 5 microns.
Still encounter a lot of resistance about this, even though the physics is very clear and known since this 1934 paper:
academic.oup.com/aje/article-ab…
Still encounter a lot of resistance about this, even though the physics is very clear and known since this 1934 paper:
academic.oup.com/aje/article-ab…
36/ Briefly, it seems like the @CDCgov confused the particles that can penetrate into the deep lung to cause tuberculosis (< 5 um) with those that fall within 1-2 um (100 um), and the error was just repeated.
This article tells the story: wired.com/story/the-teen…
This article tells the story: wired.com/story/the-teen…
37/ Inhalation, deposition, and infection
Once a susceptible person inhales a virus-containing aerosol, additional things need to happen.
- Often the aerosol will just come right back out. So to infect, it needs to deposit in the respiratory system
Once a susceptible person inhales a virus-containing aerosol, additional things need to happen.
- Often the aerosol will just come right back out. So to infect, it needs to deposit in the respiratory system

38/ Deposition depends very strongly on the size of the aerosol.
- Larger ones (> 10 um or so) cannot make the bends, and they deposit in the nose
- Smaller ones (< 10 um) often deposit in the nose too. But they can also penetrate into the bronchiolar and alveolar regions
- Larger ones (> 10 um or so) cannot make the bends, and they deposit in the nose
- Smaller ones (< 10 um) often deposit in the nose too. But they can also penetrate into the bronchiolar and alveolar regions
39/ For those interested in the history of how such a large error could persist for such a long time, this thread delves into the history:
https://twitter.com/jljcolorado/status/1391111720526024708
40/ But most people are interested in what to do to prevent transmission.
The good news is that once you accept it, explain it, and understand it, there are lots of very effective things we can do. Many are free or not very costly.
The good news is that once you accept it, explain it, and understand it, there are lots of very effective things we can do. Many are free or not very costly.
41/ We know that transmission is much lower outdoors than indoors (for COVID-19 and the flu):
(can only explain if airborne)
academic.oup.com/jid/article/22…
(can only explain if airborne)
academic.oup.com/jid/article/22…
42/ Therefore the most effective (free) thing that we can do is to meet with others outdoors whenever possible.
(No mask needed if distanced, but using masks if not distanced)
nytimes.com/2020/07/17/nyr…
(No mask needed if distanced, but using masks if not distanced)
nytimes.com/2020/07/17/nyr…

43/ If and when we have to go indoors with others, the most important thing is to explain transmission clearly:
Some (not all) infected people exhale infectious virus, which floats like smoke. We want to avoid breathing it in, or as little as possible.
Most concentrated nearby
Some (not all) infected people exhale infectious virus, which floats like smoke. We want to avoid breathing it in, or as little as possible.
Most concentrated nearby

44/ But can infect in a shared room, especially if ventilation is low. Because it can accumulate just like cigarette smoke: 
45/ Now, some people seem to think that "low ventilated spaces" are rare, and most restaurants, gyms, schools are well ventilated.
Dead wrong. Most indoor spaces are insufficiently ventilated in most countries. *Because* (in part) airborne infection was considered unusual.
Dead wrong. Most indoor spaces are insufficiently ventilated in most countries. *Because* (in part) airborne infection was considered unusual.
46/ For example, this study of 12 schools in Madrid (Spain) found that 12 out of 12 had too little ventilation, compared to what Spanish law requires for schools, and to what would be safe to reduce airborne transmission.
env-health.org/wp-content/upl…
env-health.org/wp-content/upl…

47/ And this is common also in the US, Canada, the UK, Ireland, Australia, Latin America, and really wherever people measure ventilation rates using CO2 (see #covidCO2)
We need paradigm shift to improve & increase ventilation (while not wasting energy):
science.sciencemag.org/content/372/65…
We need paradigm shift to improve & increase ventilation (while not wasting energy):
science.sciencemag.org/content/372/65…
48/ So in a location that's not very well-ventilated (you should assume that applies to you unless you know for sure otherwise) we can do 3 things:
a) Expel the air (and thus virus): ventilation
b) Keep the air, remove virus: filtration
c) Keep air + virus & try to "kill" virus
a) Expel the air (and thus virus): ventilation
b) Keep the air, remove virus: filtration
c) Keep air + virus & try to "kill" virus
49/ (a) Ventilation, expel the air outside so it carries the virus.
It works well for airborne diseases, e.g. this paper for pulmonary tuberculosis in a Taiwan college student residence. Outbreak was growing, but ended when ventilation greatly increased.
onlinelibrary.wiley.com/doi/full/10.11…
It works well for airborne diseases, e.g. this paper for pulmonary tuberculosis in a Taiwan college student residence. Outbreak was growing, but ended when ventilation greatly increased.
onlinelibrary.wiley.com/doi/full/10.11…

50/ Importantly, ventilation can be done by opening windows, so it works in low-income location.
Often don't need to open windows completely. But CRITICAL to keep them open CONTIOUOUSLY while people are there.
(typical classroom: 3 windows x 15 open all the time works)
Often don't need to open windows completely. But CRITICAL to keep them open CONTIOUOUSLY while people are there.
(typical classroom: 3 windows x 15 open all the time works)

51/ This paper has more technical details on how to ventilate to reduce airborne transmission.
sciencedirect.com/science/articl…
And we have excellent engineers that can help us do this well, e.g. you should follow @DavidElfstrom
sciencedirect.com/science/articl…
And we have excellent engineers that can help us do this well, e.g. you should follow @DavidElfstrom
52/ Approach (b). We can't ventilate enough (too cold, hot, polluted, or noisy outside, or not enough windows etc.)
Then we should filter. A filter is a medium that traps aerosols when the air flows through it.
NOT like a sieve, but through better mechanisms:
Then we should filter. A filter is a medium that traps aerosols when the air flows through it.
NOT like a sieve, but through better mechanisms:

53/ Some buildings have systems of ducts that take air from a room, pass it through a filter, send it back to the rooms
They always have a filter, typically the cheapest (MERV 8 in the US)
We should improve to MERV 13 if possible, costs a little more, works dramatically better
They always have a filter, typically the cheapest (MERV 8 in the US)
We should improve to MERV 13 if possible, costs a little more, works dramatically better

54/ As you see in the previous graph, HEPA (high efficiency particulate arrestance) filters have the highest efficiency for a single pass.
But how many aerosols we remove is the product of the flow rate of air, and that efficiency
But how many aerosols we remove is the product of the flow rate of air, and that efficiency
55/ HEPA filters have more resistance, let through less air!
Many building systems cannot tolerate HEPA, but can improve a lot by going from MERV 8 to 13
Many building systems cannot tolerate HEPA, but can improve a lot by going from MERV 8 to 13
56/ If the building doesn't have enough ventilation and filtration, we can use portable filters.
Portable HEPA units work well, but they tend to be expensive.
It is just a box with a fan and a filter (hopefully nothing else) e.g.:
Portable HEPA units work well, but they tend to be expensive.
It is just a box with a fan and a filter (hopefully nothing else) e.g.:

57/ Importantly, there is huge variation in the commercially-available filters. And a lot of people taking advantage of the pandemic to sell sub-standard products. E.g. you may pay 4 times more for a much more noisy unit of the same capacity!

https://twitter.com/marwa_zaatari/status/1374453461580873744
58/ Not all filters need to be HEPA to work! What matters is the product of the flow rate and efficiency, and once can build very useful & much cheaper filter systems with a regular (comfort) fan and a MERV13 filter:
See e.g. texairfilters.com/a-variation-on…
See e.g. texairfilters.com/a-variation-on…

59/ Approach (c): if neither ventilation or filtration are practical, then we can try to keep the air with the virus in it, but trying to "kill" the virus.
The only approach of this type that we recommend is UV disinfection.
The only approach of this type that we recommend is UV disinfection.
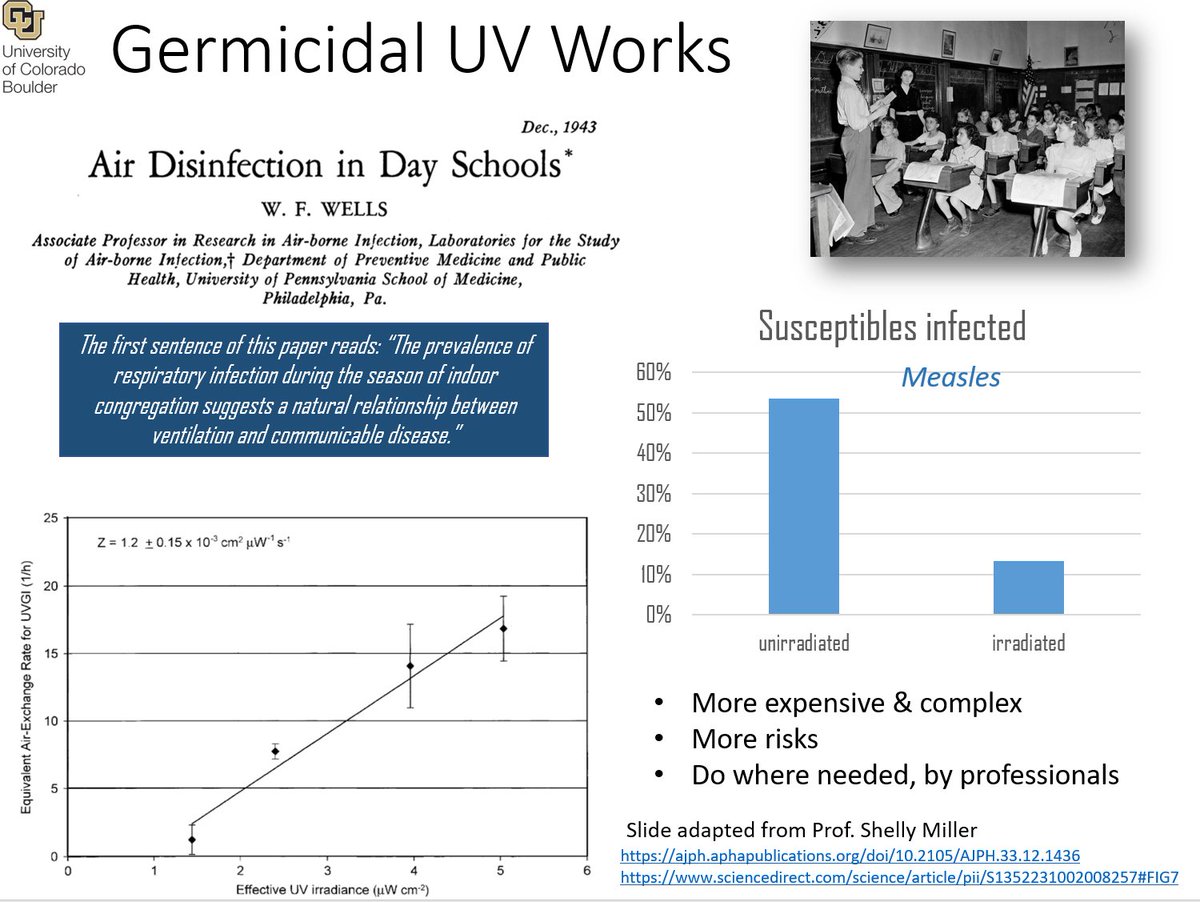
60/ Most experts prefer filtration over UV, as it is simpler and less expensive if done well.
But there is significant debate in the scientific community, some experts think that UV is underappreciated.
Just make sure to work with people with a long track record, if you go UV
But there is significant debate in the scientific community, some experts think that UV is underappreciated.
Just make sure to work with people with a long track record, if you go UV
61/ Now we come to the other types of approaches to keep the air and the virus, but "kill the virus"
They all try to do this through chemical reactions of chemical species (that they introduce into the air) and the virus molecules.
We do NOT recommend them!
They all try to do this through chemical reactions of chemical species (that they introduce into the air) and the virus molecules.
We do NOT recommend them!

62/ There are two reasons why we do NOT recommend electronic air cleaners (ions, plasmas, photocatalysis, hydroxyl) or spraying ozone, hypochlorous acid, chlorine dioxide, hydrogen peroxide, alcohol into the air.
63/ - First, the chemical reactions that may destroy the virus, do so by chemical reactions with the virus molecules, which are... proteins, lipids, and nucleic acids
But if people are in that air, they are made of... proteins, lipids, and nucleic acids!! Chemicals hurt them too
But if people are in that air, they are made of... proteins, lipids, and nucleic acids!! Chemicals hurt them too
64/ - Second, the chemicals produced by these systems often react with volatile organic compounds (which are abundant indoors) and turn them into more toxic chemicals, or chemical aerosols which are also toxic.
E.g. see this paper: pubs.acs.org/doi/10.1021/ac…
E.g. see this paper: pubs.acs.org/doi/10.1021/ac…
65/ For more details on air cleaners, see this thread. It is from a year ago, but completely relevant.
https://twitter.com/jljcolorado/status/1337073578345435138
66/ Another approach to breathe in less virus ("like smoke") is to wear a mask.
No matter what the antimaskers will tell you, masks work to remove virus-laden aerosols.
Masks are definitely annoying, but getting COVID or passing it along is a lot more "annoying"
No matter what the antimaskers will tell you, masks work to remove virus-laden aerosols.
Masks are definitely annoying, but getting COVID or passing it along is a lot more "annoying"

67/ Three things are important for masks:
- Good quality filter, that removes aerosols when the air goes through
- Low pressure drop, so that we can breathe easily through them
- Fit well to the face, not leaving any gaps
Any mask will help, but variation is huge:
- Good quality filter, that removes aerosols when the air goes through
- Low pressure drop, so that we can breathe easily through them
- Fit well to the face, not leaving any gaps
Any mask will help, but variation is huge:

68/ Personally I recommend elastomeric N95 masks
- Use N95 filter, so have good efficiency & breathability
- They improve upon the part that N95 masks don't do well, which is having a very good fit to the face
E.g. envomask.com is the one I use (come w/ valve plug)
- Use N95 filter, so have good efficiency & breathability
- They improve upon the part that N95 masks don't do well, which is having a very good fit to the face
E.g. envomask.com is the one I use (come w/ valve plug)

69/ We wrote a letter to @CDCgov and the Biden administration in Feb., asking them to invoke the Defense Production Act to make and distribute better masks.
Unfortunately they were only focused on the vaccine, which has not been enough.
drive.google.com/drive/u/0/fold…
Unfortunately they were only focused on the vaccine, which has not been enough.
drive.google.com/drive/u/0/fold…
70/ What measures should we stop?
We should continue to distance (breathe less exhaled "smoke" from others) and wash our hands (as a precaution, and bc of other pathogens)
Should STOP hygiene theatre of surface disinfection. Doesn't help, cost $$, gives false sense of security
We should continue to distance (breathe less exhaled "smoke" from others) and wash our hands (as a precaution, and bc of other pathogens)
Should STOP hygiene theatre of surface disinfection. Doesn't help, cost $$, gives false sense of security

71/ We should keep plexiglass barriers in a cashier or teller situation, but get rid of them in "lateral" situations in offices or schools:
Not only they don't help, they INCREASE transmission by trapping the air!
dx.doi.org/10.1126/scienc…
Not only they don't help, they INCREASE transmission by trapping the air!
dx.doi.org/10.1126/scienc…

72/ One thing I forgot above when I was talking about ventilation, is that we can use affordable ($100) or so NDIR (infrared) CO2 meters to see if a location is well ventilated enough.
- Outdoor air ~ 420 ppm (parts per million)
- Our breath ~ 40000
- Well ventilated < 700
- Outdoor air ~ 420 ppm (parts per million)
- Our breath ~ 40000
- Well ventilated < 700
73/ Poorly ventilated locations often have many thousands of ppm, such as the Spanish schools I mentioned above. 

74/ Every public place should have a display of CO2, which is cheap to do.
This was law before the pandemic is Taiwan and South Korea, has become law in e.g. Belgium and some parts of Spain (for some locations in all cases). Should extend everywhere:
This was law before the pandemic is Taiwan and South Korea, has become law in e.g. Belgium and some parts of Spain (for some locations in all cases). Should extend everywhere:

75/ I could go on and on, but I trust whoever has made it all the way here is tired of reading.
More details and links on these topics on my slide deck at: Bit.ly/COVID-Aerosols3
More details and links on these topics on my slide deck at: Bit.ly/COVID-Aerosols3
77/ And great people to follow include @linseymarr @kprather88 @lisa_iannattone @JenniferKShea @CorsIAQ @HuffmanLabDU @ShellyMBoulder @ChemDelphine @DFisman @DavidElfstrom @WBahnfleth @Poppendieck @CPita3 and many others
The thread continues here, I made a mistake and have two tweets labeled 26 that bifurcate:
https://twitter.com/jljcolorado/status/1430981281404313608
78/ Hare una version en español de este hilo, seguramente este fin de semana
70/ La versión en español está en 2 hilos separados el primero para la ciencia y el segundo para la prevención.
Este es el de la ciencia:
Este es el de la ciencia:
https://twitter.com/jljcolorado/status/1431755596387209222?s=19
• • •
Missing some Tweet in this thread? You can try to
force a refresh










