The last few weeks have been tough. For those in need of a light hearted thread, here’s a brand new 3rd #tweetorial in my extremes of #physiology series. What can the animal kingdom teach us about our physiology?
Buckle up for some fun animal pulmonary facts 🫁!
1/
Buckle up for some fun animal pulmonary facts 🫁!
1/
CASE 1:
You are performing a bronchoscopy. Upon reaching the main carina instead of the usual TWO airways (right & left mainstem bronchi) you see THREE.
Your assistant says “Whoa! That’s weird”
You say no it’s totally normal because the patient is a:
2/
You are performing a bronchoscopy. Upon reaching the main carina instead of the usual TWO airways (right & left mainstem bronchi) you see THREE.
Your assistant says “Whoa! That’s weird”
You say no it’s totally normal because the patient is a:
2/
Answer: 🐖
In pigs, the RUL lobe bronchus originates from the supra-carinal trachea (e.g. before the R & L mainstream branches). The view from the trachea looks like this (see the tracheal bronchus on the right).
image source: casereports.bmj.com/content/12/5/e…
3/

In pigs, the RUL lobe bronchus originates from the supra-carinal trachea (e.g. before the R & L mainstream branches). The view from the trachea looks like this (see the tracheal bronchus on the right).
image source: casereports.bmj.com/content/12/5/e…
3/


Clinical 🥡:
~1% of humans have a tracheal bronchus as an anatomical variant (usually RUL).
This trachea bronchus can cause RUL collapse when intubated.
So if you have an intubated patient with unexplained RUL collapse always think - could this person have a 🐖 bronchus?
4/


~1% of humans have a tracheal bronchus as an anatomical variant (usually RUL).
This trachea bronchus can cause RUL collapse when intubated.
So if you have an intubated patient with unexplained RUL collapse always think - could this person have a 🐖 bronchus?
4/



Other answers:
🦒, 🐑, 🐐, 🐪, & 🐋 also have tracheal bronchi but I don’t think anyone has done a bronch on a 🦒!
It is possible to do bronchoscopy in 🐘 - though not easy! A trunk nerve block apparently works better than nasal lidocaine gel. 🐘 don’t have tracheal bronchi.
5/


🦒, 🐑, 🐐, 🐪, & 🐋 also have tracheal bronchi but I don’t think anyone has done a bronch on a 🦒!
It is possible to do bronchoscopy in 🐘 - though not easy! A trunk nerve block apparently works better than nasal lidocaine gel. 🐘 don’t have tracheal bronchi.
5/



Case 2:
You have just placed a LEFT sided chest tube for a patient with large BILATERAL pneumothoraces. Your assistant asks you if you want to place a second tube on the RIGHT side.
You say no, the procedure is unnecessary because the patient is a:
6/
You have just placed a LEFT sided chest tube for a patient with large BILATERAL pneumothoraces. Your assistant asks you if you want to place a second tube on the RIGHT side.
You say no, the procedure is unnecessary because the patient is a:
6/
Answer: 🦬
The American Buffalo has a single pleural cavity. Despite its size (up to 2600 lbs) & speed (runs up to 40 mph) a single arrow can cause bilateral tension PTX, incapacitating the buffalo.
(Aside: note that the Plains bison has one of the best species names ever!)
7/
The American Buffalo has a single pleural cavity. Despite its size (up to 2600 lbs) & speed (runs up to 40 mph) a single arrow can cause bilateral tension PTX, incapacitating the buffalo.
(Aside: note that the Plains bison has one of the best species names ever!)
7/

1st Clinical 🥡:
People who have had thoracic surgery that disrupts the pleura, may also have a single pleural space, just like a Buffalo.
(It can also occur rarely in the absence of thoracic surgery as an anatomical variant).
8/
Source: NEJM nejm.org/doi/10.1056/NE…
People who have had thoracic surgery that disrupts the pleura, may also have a single pleural space, just like a Buffalo.
(It can also occur rarely in the absence of thoracic surgery as an anatomical variant).
8/
Source: NEJM nejm.org/doi/10.1056/NE…

2nd Clinical 🥡:
This is why in lung transplant recipients a single transbronchial biopsy can cause bilateral PTX.
It's also why, in rare cases, a single chest tube may suffice to treat bilateral PTX.
9/
jhltonline.org/article/S1053-… pubmed.ncbi.nlm.nih.gov/16714521/

This is why in lung transplant recipients a single transbronchial biopsy can cause bilateral PTX.
It's also why, in rare cases, a single chest tube may suffice to treat bilateral PTX.
9/
jhltonline.org/article/S1053-… pubmed.ncbi.nlm.nih.gov/16714521/


Other answers:
🐖 pleural anatomy is similar to humans, other than tracheal bronchi
🐘It’s impossible to place a chest tube in an elephant! (more on this later)
Some 🐍 also have one pleural space but for a very different reason: they only have one 🫁
vetexotic.theclinics.com/article/S1094-…
10/

🐖 pleural anatomy is similar to humans, other than tracheal bronchi
🐘It’s impossible to place a chest tube in an elephant! (more on this later)
Some 🐍 also have one pleural space but for a very different reason: they only have one 🫁
vetexotic.theclinics.com/article/S1094-…
10/

CASE 3:
You are performing transbronchial biopsies when (oh no!) you realize that your last biopsy appears to have gotten a bite of pleura.
Horrified your assistant asks if you need a chest tube tray.
“No" you say reassuringly, it's unnecessary because the patient is a ___.
11/
You are performing transbronchial biopsies when (oh no!) you realize that your last biopsy appears to have gotten a bite of pleura.
Horrified your assistant asks if you need a chest tube tray.
“No" you say reassuringly, it's unnecessary because the patient is a ___.
11/
Answer: 🐘 Elephant
Elephants are the *ONLY* mammal that does not have a pleural space. In utero their visceral & parietal pleura fuse, obliterating the pleural space with dense connective tissue.
Thus elephants can’t develop PTX (and its impossible to place a chest tube)!
12/
Elephants are the *ONLY* mammal that does not have a pleural space. In utero their visceral & parietal pleura fuse, obliterating the pleural space with dense connective tissue.
Thus elephants can’t develop PTX (and its impossible to place a chest tube)!
12/
But *WHY* are 🐘's pleural cavities unique?
The answer is that elephants snorkel to cross deep water. This creates massive negative intra-pleural pressure, which would in another species cause massive fluid transudation. 🐘 natural pleurodesis enables them to tolerate this.
13/

The answer is that elephants snorkel to cross deep water. This creates massive negative intra-pleural pressure, which would in another species cause massive fluid transudation. 🐘 natural pleurodesis enables them to tolerate this.
13/
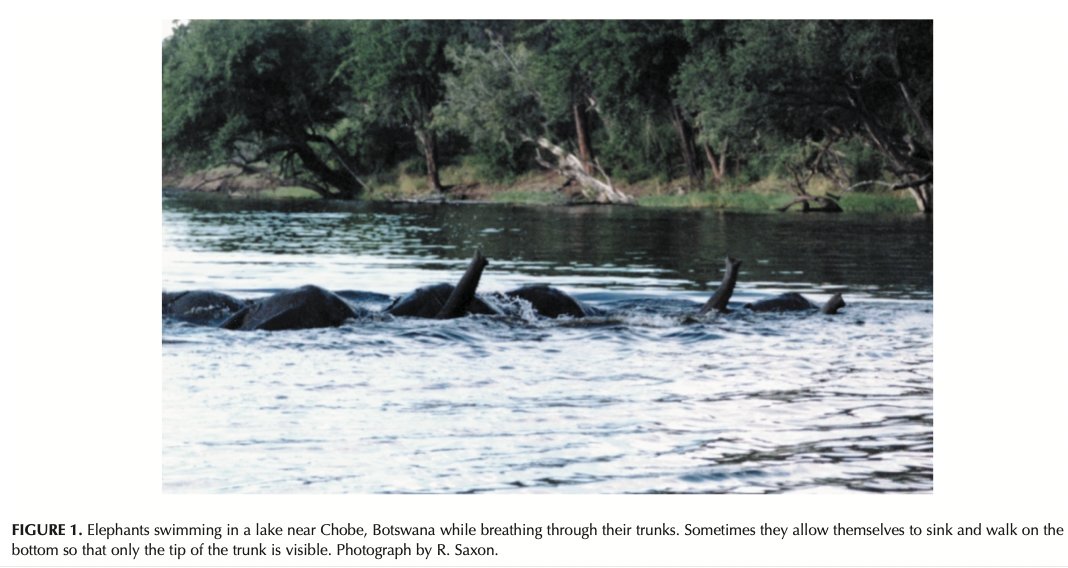

I *HIGHLY* recommend reading this excellent article by West about the unique physiologic adaptations that enable elephant snorkeling 🐘🤿
Another fun fact: their diaphragms are 3 cm thick (10x ours), enabling them to pull negative pressure underwater
pubmed.ncbi.nlm.nih.gov/11311306/
14/
Another fun fact: their diaphragms are 3 cm thick (10x ours), enabling them to pull negative pressure underwater
pubmed.ncbi.nlm.nih.gov/11311306/
14/

Clinical 🥡:
Humans who undergo pleurodesis are protected against pneumothorax; in some cases this is why the procedure is performed. In one case series of patients with primary spontaneous PTX, talc pleurodesis prevented recurrent PTX in 95% of them.
erj.ersjournals.com/content/29/4/7…
15/
Humans who undergo pleurodesis are protected against pneumothorax; in some cases this is why the procedure is performed. In one case series of patients with primary spontaneous PTX, talc pleurodesis prevented recurrent PTX in 95% of them.
erj.ersjournals.com/content/29/4/7…
15/
Other answers:
🐃 Buffalo - PTX are a huge deal in buffalos because they are always bilateral! (see case 2)
🐪 & 🦏 can also develop PTX
Cetacean lungs have abnormally high compliance so they can take *HUGE* tidal volumes (a🐬's TV is 55 ml/kg); even🐬 can develop PTX rarely
14/
🐃 Buffalo - PTX are a huge deal in buffalos because they are always bilateral! (see case 2)
🐪 & 🦏 can also develop PTX
Cetacean lungs have abnormally high compliance so they can take *HUGE* tidal volumes (a🐬's TV is 55 ml/kg); even🐬 can develop PTX rarely
14/

CASE 4:
You are called from the PFT lab about an abnormal CPET result: VO2max 255 ml/kg·min
The technicians says this calculation can’t possibly be right. You tell them it’s expected because the patient is a ____
15/
You are called from the PFT lab about an abnormal CPET result: VO2max 255 ml/kg·min
The technicians says this calculation can’t possibly be right. You tell them it’s expected because the patient is a ____
15/
Wrong answers first:
🥇 The highest recorded human VO2max was 97.5 mL/kg/min (set by 🇳🇴 cyclist Oskar Svedsen in 2012)
For comparison, the average in a sedentary non-professional athlete is about 30-40 mL/kg/min (men) and 27-35 mL/kg/min (women).
16/
🥇 The highest recorded human VO2max was 97.5 mL/kg/min (set by 🇳🇴 cyclist Oskar Svedsen in 2012)
For comparison, the average in a sedentary non-professional athlete is about 30-40 mL/kg/min (men) and 27-35 mL/kg/min (women).
16/
🐎 Thoroughbred horses running on an inclined treadmill averaged 194 mL/kg/min after 18 weeks of high intensity training (yes horses do HIT classes!)
According to a colleague, the sound made by a horse’s hooves running on a treadmill was deafening!
physoc.onlinelibrary.wiley.com/doi/full/10.11…
17/

According to a colleague, the sound made by a horse’s hooves running on a treadmill was deafening!
physoc.onlinelibrary.wiley.com/doi/full/10.11…
17/


Huskies from a champion dogsled team have demonstrated VO2max as high as 240 ml/kg/min.
The dogs who run the 938 mile Iditerod in just 8 days are perhaps the best endurance athletes in the world.
news.cornell.edu/stories/1996/1…
18/

The dogs who run the 938 mile Iditerod in just 8 days are perhaps the best endurance athletes in the world.
news.cornell.edu/stories/1996/1…
18/


🐁 The tiny 10 gm Pygmy Mouse achieves an incredible VO2max >250 ml/kg/min.
This is a great demonstration of allometric scaling laws at work: smaller animals have much denser mitochondria enabling greater VO2; this is also why they have higher BMR/mass
general.utpb.edu/fac/eldridge_j…
19/

This is a great demonstration of allometric scaling laws at work: smaller animals have much denser mitochondria enabling greater VO2; this is also why they have higher BMR/mass
general.utpb.edu/fac/eldridge_j…
19/


Answer: 🐦
The real champion is the 4 gm hummingbird, with a VO2max of >660 ml/kg/min.
This is close to the theoretical limit of what is possible (e.g. their muscle cells are so dense that adding more mitochondria would take away sarcomeres!)
pnas.org/content/88/11/…
20/
The real champion is the 4 gm hummingbird, with a VO2max of >660 ml/kg/min.
This is close to the theoretical limit of what is possible (e.g. their muscle cells are so dense that adding more mitochondria would take away sarcomeres!)
pnas.org/content/88/11/…
20/

If you are wondering *HOW* they measure the VO2max of a 4 gm hummingbird, they get the birds to insert their beak into a feeder while hovering and measure the CO2 and O2 concentration.
utsc.utoronto.ca/news-events/br…
21/
utsc.utoronto.ca/news-events/br…
21/

If you like this, I highly recommend reading this amazingly detailed Quora thread. Just fantastic.
Highlights: hummingbirds VO2max is >1000 ml/kg/min if they fly in thin air (He/O2 mix); IMO this is cheating, like hitting golf balls on the moon.
quora.com/Whats-the-high…
22/
Highlights: hummingbirds VO2max is >1000 ml/kg/min if they fly in thin air (He/O2 mix); IMO this is cheating, like hitting golf balls on the moon.
quora.com/Whats-the-high…
22/
Clinical 🥡:
Elite athletes can have a VO2max that’s ~3x “average.” When evaluating for change in exercise tolerance it’s important to think about what their baseline was; e.g. going from 60 to 40 could be a big drop but still be “normal” range.
Also we got nothing on 🐦!
23/
Elite athletes can have a VO2max that’s ~3x “average.” When evaluating for change in exercise tolerance it’s important to think about what their baseline was; e.g. going from 60 to 40 could be a big drop but still be “normal” range.
Also we got nothing on 🐦!
23/
Hope you’ve enjoyed the 3️⃣rd installment in this series. Hopefully you’ve learned something that will make you a better doctor, or at least increase your enjoyment of the discovery channel.
For earlier installments see:
1️⃣
2️⃣
24/
For earlier installments see:
1️⃣
https://twitter.com/nickmmark/status/1346589425938010112?s=20
2️⃣
https://twitter.com/nickmmark/status/1352335092350238721?s=20
24/
• • •
Missing some Tweet in this thread? You can try to
force a refresh
































