
This #novice thread is all about inhaled anaesthetic agents (Volatiles)
It starts with a detailed infographic, which we will break down as we go along.
I’ve linked some resources that are worth exploring (for other content as well beyond this thread)
Comments welcome!
1/n
It starts with a detailed infographic, which we will break down as we go along.
I’ve linked some resources that are worth exploring (for other content as well beyond this thread)
Comments welcome!
1/n

I want to recommend this YouTube channel from @UKAnesth Randall Schell has made lots of videos and they are very exam focused and comprehensive. So have a watch while exercising or commuting...
2/n
2/n
Also 2 good @accracpodcast episodes to listen to
accrac.com/episode-1-prop…
accrac.com/episode-193-ke…
3/n
accrac.com/episode-1-prop…
accrac.com/episode-193-ke…
3/n
The inhaled agents are the oldest anaesthetic agents. N2O was used for dental anaesthesia by Horace Wells in 1842 and Ether by William Morton famously on 16 October 1846 (“Ether Day”). Horace Wells’ story is tragic
dx.doi.org/10.1016%2FS037…
4/n
dx.doi.org/10.1016%2FS037…
4/n

The precise mechanism of action for these anaesthetics is unknown. But is probably through action on specific membrane ion channels associated with certain neurotransmitters (e.g GABA). A nice review is found here
doi.org/10.1016/B978-0…
and doi.org/10.1056/nejmra…
5/n
doi.org/10.1016/B978-0…
and doi.org/10.1056/nejmra…
5/n

To achieve anaesthesia the drugs most probably act on spinal cord, amygdala, hippocampus, cortex and thalamus. These structures would be involved in analgaesia, hypnosis, amnesia and immobility
6/n
6/n
We don’t know the mechanism…is it working?
We use the Minimum Alveolar Concentration (MAC)…which has been calculated for each agent and tells us the concentration of anaesthetic needed to prevent response to surgical stimulus in 50% of people
doi.org/10.1093/bja/ae…
7/n
We use the Minimum Alveolar Concentration (MAC)…which has been calculated for each agent and tells us the concentration of anaesthetic needed to prevent response to surgical stimulus in 50% of people
doi.org/10.1093/bja/ae…
7/n
MAC is derived from the end-expired concentration. This is used because it reflects alveolar concentration, which in turn reflects arterial concentration which in term reflects brain parenchymal concentration
When we say concentration…we are talking about partial pressures
8/n
When we say concentration…we are talking about partial pressures
8/n
MAC can be affected by agents that aren’t measured in the end tidal stream…
- IV agents,
- the patient chemical milieu (acid-base status, thyroid function, temperature)
- or demographics (Age, pregnancy).
So the ET MAC reading has to be interpreted in context
9/n
- IV agents,
- the patient chemical milieu (acid-base status, thyroid function, temperature)
- or demographics (Age, pregnancy).
So the ET MAC reading has to be interpreted in context
9/n
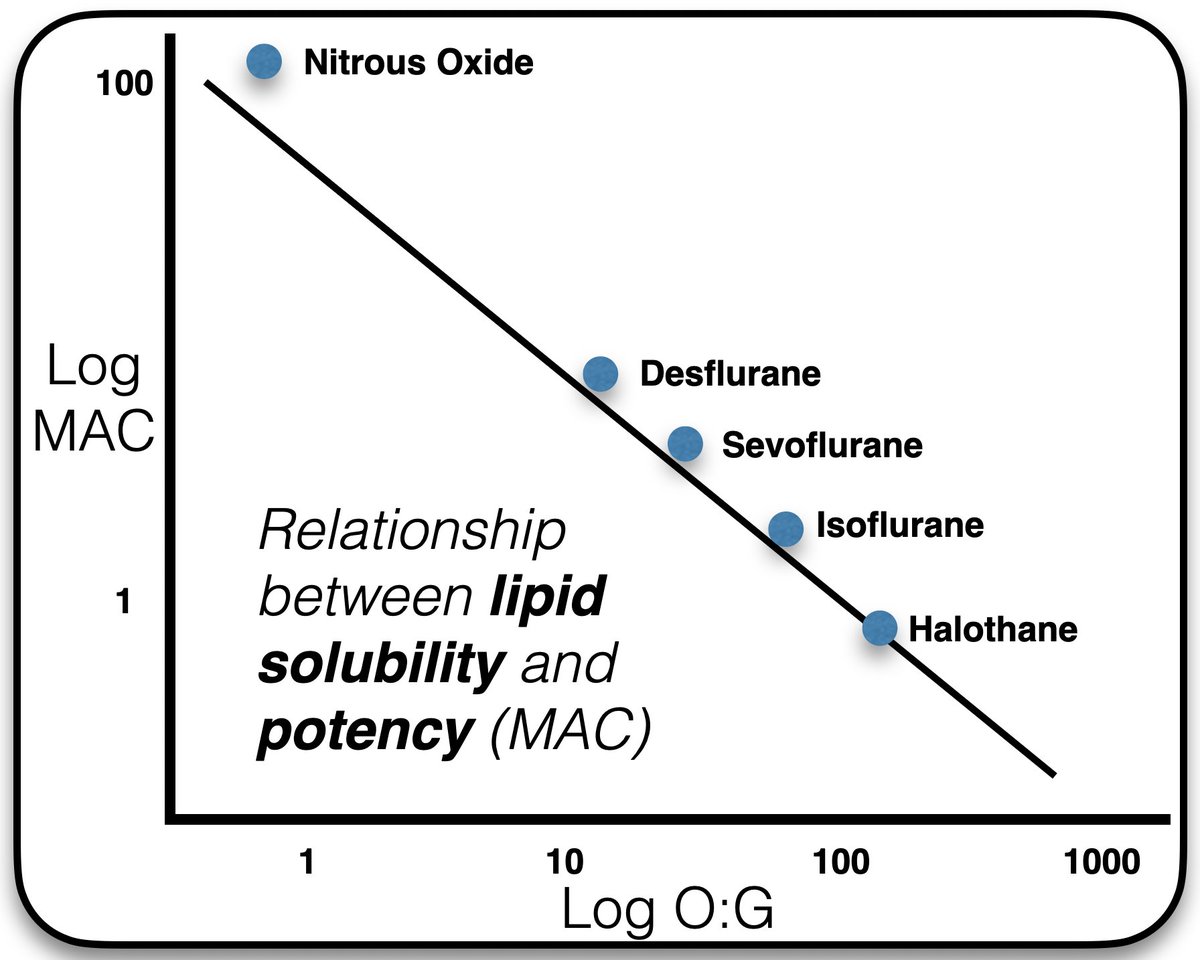
The MAC is synonymous with potency…I.e what concentration is needed for same effect. This correlates most closely with the lipid solubility (oil:gas ratio)
10/n
10/n
The commonest agents still in use (UK) are Nitrous Oxide, Sevoflurane, Desflurane, Isoflurane.
Only N2O is a “gas”. The other agents are considered “vapours” because they exist in liquid and gaseous phase at STP.
11/n
Only N2O is a “gas”. The other agents are considered “vapours” because they exist in liquid and gaseous phase at STP.
11/n
So we package our volatiles into a delivery device (vaporiser) which delivers an agent via the anaesthetic machine at a given concentration to the patient. We can measure this dose in the brain using end tidal concentration as a surrogate. This is medicolegally robust.
12/n
12/n
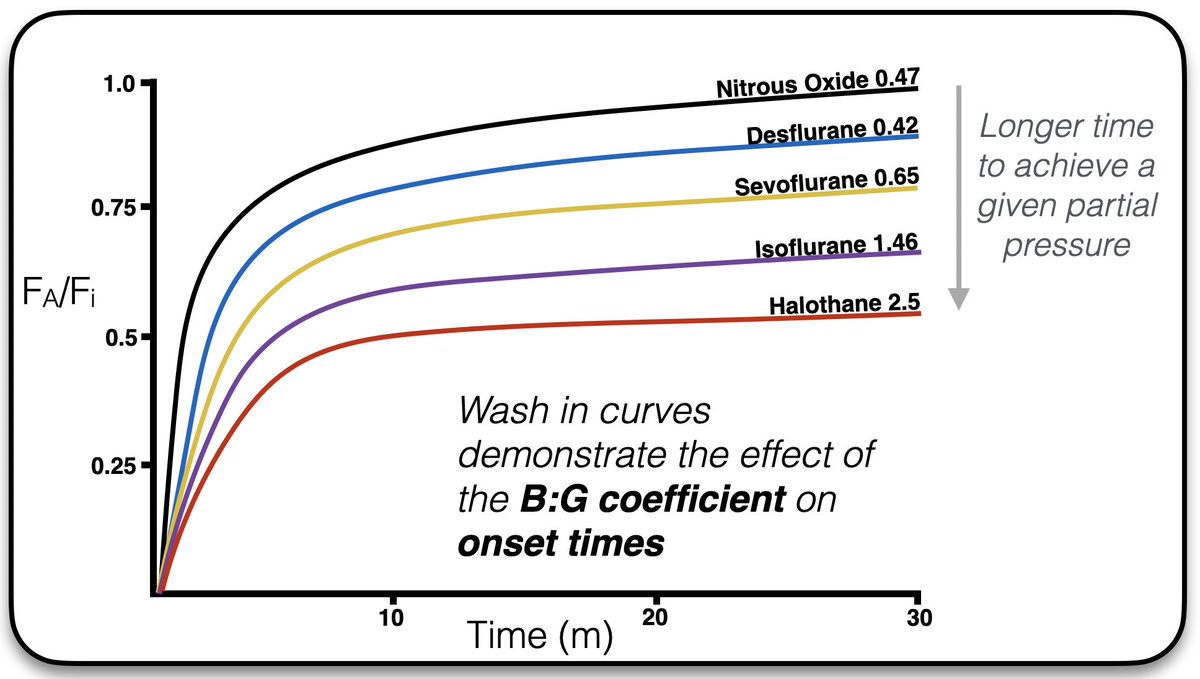
In order to quickly achieve a desired partial pressure in the brain (=anaesthesia), we want an agent that is poorly soluble (hence most of the agent is exerting a partial pressure rather than dissolved and inert)
A low blood:gas solubility is desirable for quick anaesthesia.
13/n
A low blood:gas solubility is desirable for quick anaesthesia.
13/n
We have to get the agent into the blood stream quickly…Which requires a high concentration in the alveoli.
The gradient is maximised by
-Low FRC
-Increased minute ventilation
-Increased inspired concentration
-Low cardiac output
-“Concentration effect”
-“Second gas effect”
14/n
The gradient is maximised by
-Low FRC
-Increased minute ventilation
-Increased inspired concentration
-Low cardiac output
-“Concentration effect”
-“Second gas effect”
14/n
The second gas effect occurs when N2O diffuses rapidly out of alveoli. This causes a pressure gradient with the conducting airway and encourages flow into it the alveoli. This flow brings with it the other (second) gas being administered.
15/n
15/n
As this second gas is brought into the alveoli it’s relative concentration increases (since he N2O has diffused out) and we see the concentration effect
16/n
16/n
Maintaining high alveolar partial pressure will facilitate rapid induction of anaesthesia and we can plot wash-in curves demonstrating the agents that most rapidly reach an alveolar concentration similar to the inspired concentration (and therefore high enough)
17/n
17/n
To end, I want to highlight that the volatile anaesthetics are extremely bad for the environment.
doi.org/10.1111/anae.1…
You can see the impact here rcoa.ac.uk/about-college/…
18/n
doi.org/10.1111/anae.1…
You can see the impact here rcoa.ac.uk/about-college/…
18/n

We can mitigate this effect with low flows, depth of anaesthesia monitoring, adjuvant treatments and choosing the least bad volatile. 19/n
• • •
Missing some Tweet in this thread? You can try to
force a refresh





