🔥Hot Take🔥
Are we approaching blood pressure measurement wrong in primary care?
Maybe we need to check BP less often?
Here is my pitch...
A #hypertension thread that might raise your BP
Are we approaching blood pressure measurement wrong in primary care?
Maybe we need to check BP less often?
Here is my pitch...
A #hypertension thread that might raise your BP

Central thesis
Measurement overload contributes to clinician inertia AND patient skepticism about elevated BP diagnosis.
What if we reoriented BP measurement to be a high-quality ANNUAL screening instead of a poor-quality measure done at every single office visit?
Measurement overload contributes to clinician inertia AND patient skepticism about elevated BP diagnosis.
What if we reoriented BP measurement to be a high-quality ANNUAL screening instead of a poor-quality measure done at every single office visit?
Key question
Why do we check BP at every clinic visit?
Why do we check BP at every clinic visit?
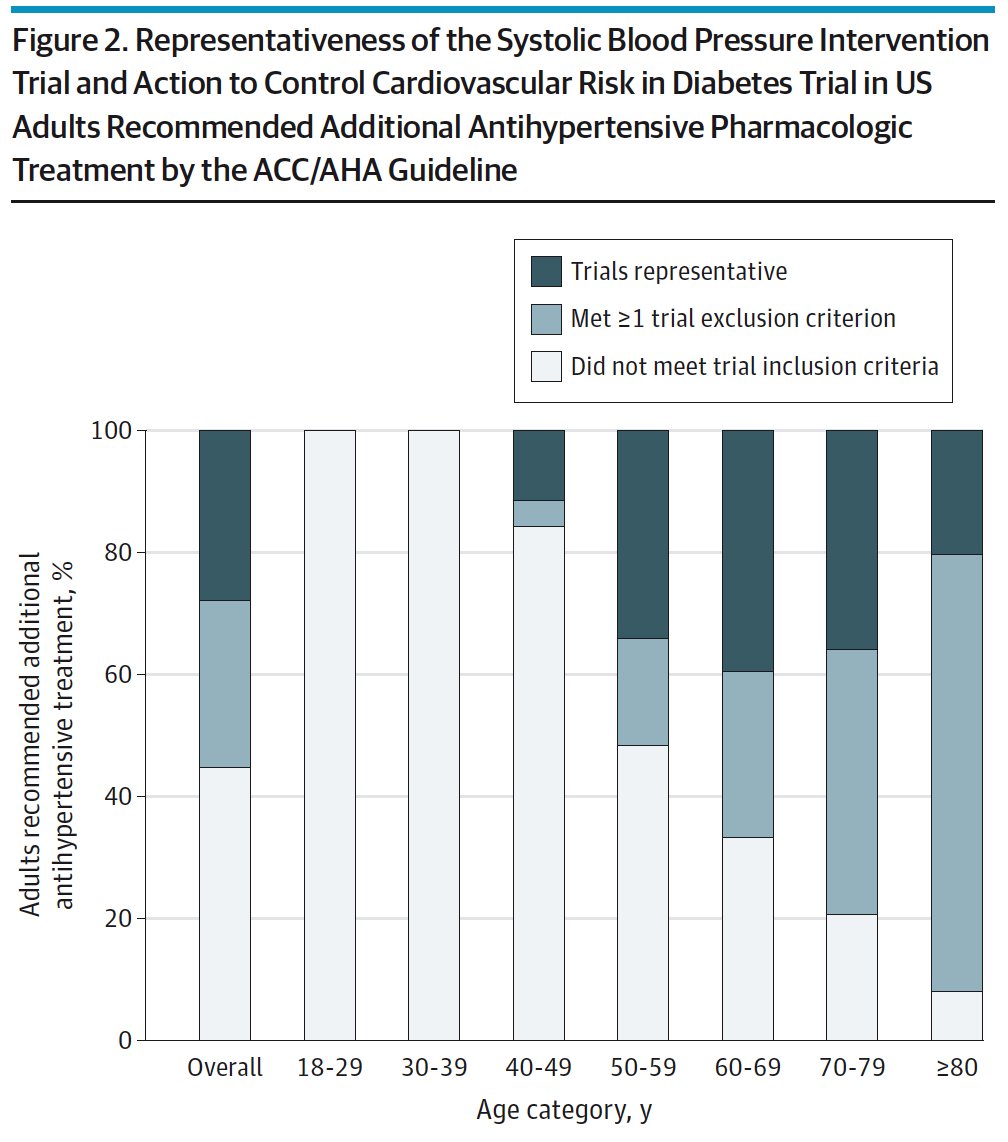
Hypertension is a huge, long-term, public health problem.
It is clear that we both underdiagnose and undertreat it.
jamanetwork.com/journals/jama/…
It is clear that we both underdiagnose and undertreat it.
jamanetwork.com/journals/jama/…
One (of many) barriers to HTN control is that BP measurement is challenging.
Office BPs, in the real-world, are often done incorrectly and may not represent steady state when performed on patients in clinic for acute illnesses.
Also, BP is not the focus of most PCP visits.
Office BPs, in the real-world, are often done incorrectly and may not represent steady state when performed on patients in clinic for acute illnesses.
Also, BP is not the focus of most PCP visits.
For example, what am I supposed to do with a set of 10 clinic BPs ranging 110s-140s/60-80s for one of my primary care patients all taken for visits for other reasons in 1 year?
My #hypertension friends push that we need better BP techniques.
I agree, but best practice office BPs take 5-15 min….requiring multiple spaced readings after 5 minutes of rest
jamanetwork.com/journals/jama/…
I agree, but best practice office BPs take 5-15 min….requiring multiple spaced readings after 5 minutes of rest
jamanetwork.com/journals/jama/…
Sorry friends, but even if made optimally efficient (see link), this will not fit into a primary care workflow with 20 min visits & exam rooms at capacity.
At least not for every visit!
pubmed.ncbi.nlm.nih.gov/34488436/
At least not for every visit!
pubmed.ncbi.nlm.nih.gov/34488436/
The other big pushes - home & ambulatory BP monitoring are both good...
...but asking every patient with a BP of 130/80 to buy a home cuff or wear an ABPM is asking a lot. Carries a time and $ cost to patients + increased worry.
...but asking every patient with a BP of 130/80 to buy a home cuff or wear an ABPM is asking a lot. Carries a time and $ cost to patients + increased worry.
So, remind me, why do we check BP at every visit?
1.It is a vital sign
2.To find hypotension
3.To screen for hypertension
4. Docs love numbers
1.It is a vital sign
2.To find hypotension
3.To screen for hypertension
4. Docs love numbers
1/2 Vital sign / find hypotension
Sure, but we don’t check temps on all patients. We have protocols to check based on certain symptoms. I don’t see a reason that this can’t be done for BP as well.
We need to separate the concepts of BP as a diagnostic vs screening tool
Sure, but we don’t check temps on all patients. We have protocols to check based on certain symptoms. I don’t see a reason that this can’t be done for BP as well.
We need to separate the concepts of BP as a diagnostic vs screening tool
3. To screen for hypertension
We screen for cholesterol and diabetes annually (or less).
Why don’t we do this for BP?
In fact, USPSTF recommends only annual BP screening for age >40 & every 3-5 years for young/low risk pops…
jamanetwork.com/journals/jama/…
We screen for cholesterol and diabetes annually (or less).
Why don’t we do this for BP?
In fact, USPSTF recommends only annual BP screening for age >40 & every 3-5 years for young/low risk pops…
jamanetwork.com/journals/jama/…
So let’s imagine a world with a new approach…
For annual / new pt visits: Patients always gets a high-quality, rested, quiet room, multiple reading office screening BP. (Time invested)
If BP is newly elevated, they get set up with ABPM or home cuff...
For annual / new pt visits: Patients always gets a high-quality, rested, quiet room, multiple reading office screening BP. (Time invested)
If BP is newly elevated, they get set up with ABPM or home cuff...
When they come in later on for a knee injury, WE DO NOT CHECK A BP. (Time saved)
When they come in later on for fever and cough, we check *diagnostic* BP
In the EHR, we make it clear that each BP is either screening or diagnostic.
When they come in later on for fever and cough, we check *diagnostic* BP
In the EHR, we make it clear that each BP is either screening or diagnostic.
For my patient with known HTN at goal, we also only do a formal BP reading annually (perhaps they monitor at home).
We again don’t check a BP for acute visits unless related to specific symptoms.
We again don’t check a BP for acute visits unless related to specific symptoms.
For my patient with known HTN above goal, we do formal checks at annual visits & we schedule actual HTN follow up visits.
We stop pretending BP management is something we can effectively add on as the 6th item on a visit for other acute concerns.
We stop pretending BP management is something we can effectively add on as the 6th item on a visit for other acute concerns.
Would this not simplify things for patients/docs/staff?
Appreciate any/all critique, feedback, evidence this argument has been made before or that it won’t work.
Appreciate any/all critique, feedback, evidence this argument has been made before or that it won’t work.
Note that this set of thoughts skips over the (much more important) upstream issue of access to primary care in the first place, which is beyond that of HTN.
I'm assuming we've fixed that tiny problem
jamanetwork.com/journals/jamai…
I'm assuming we've fixed that tiny problem
jamanetwork.com/journals/jamai…
Sorry for the long thread!
@ThreadReaderApp unroll for an easier to read format
@ThreadReaderApp unroll for an easier to read format
• • •
Missing some Tweet in this thread? You can try to
force a refresh